Ultrasound diagnosis of common musculo-skeletal disorders in young athletes – Part I
Pierre Vassallo
U ltrasound (US) has become the most commonly used imaging method to assess musculo-skeletal (MSK) injuries. In addition to the high soft tissue image quality it provides, MSK US has the advantage of providing a rapid mode of evaluation that avoids the use of ionising radiation, allows dynamic assessment and can guide targeted treatment. Use of high quality scanning equipment to diagnose and treat MSK injuries is of the utmost importance. Without the necessary high image resolution, most injuries will be missed. Sonographer experience also has a major influence on diagnostic accuracy.
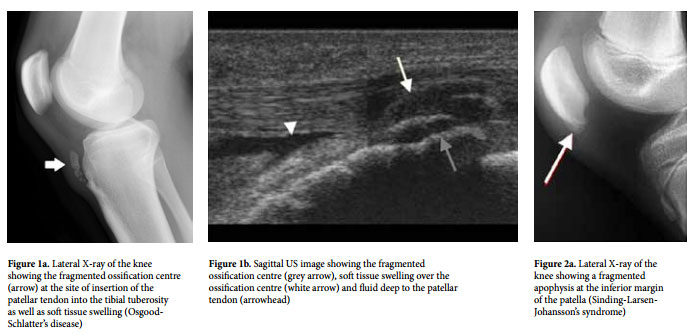
In children, tendons and ligaments are usually stronger than the growth plate. Thus, growth plate injuries are more common than tendonous/ligamentous injuries. Consequently, overuse injuries in a tendon that attaches to an un-united apophysis are more likely to affect the apophysis than the tendon. Such injuries were previously referred to as osteochondrites or apophysites, however they are now recognised as overuse injuries. The most common type of apophyseal overuse injury is Osgood-Schlatter’s disease (OSD), which affects the insertion of the patellar tendon into the tibia. In the past, a child or young adult presenting with pain below the patella would promptly be referred for a lateral X-ray of the knee (Fig 1a) to detect OSD. Today, an ultrasound of the knee will not only depict the fragmented ossification centre seen on X-ray, but will also provide more detailed information on the state of the soft tissues, including the presence of any fluid collections or adventitial bursae, while confirming or otherwise the integrity of the patellar tendon (Fig 1b).
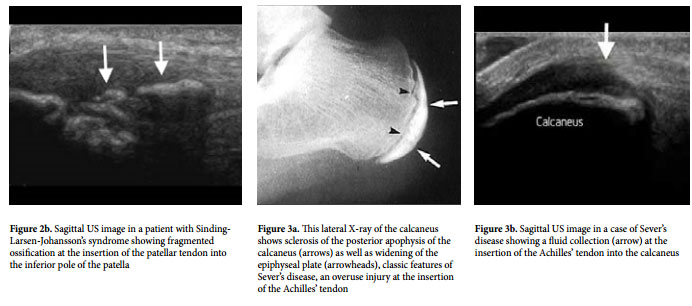
Other common sites of apophyseal injury include the proximal patellar tendon insertion (Sinding-Larsen-Johansson’s disease) (Fig 2), the insertion of the Achilles’ tendon into the calcaneus (Sever’s disease) (Fig 3) and the insertion of the triceps muscle into the olecranon.
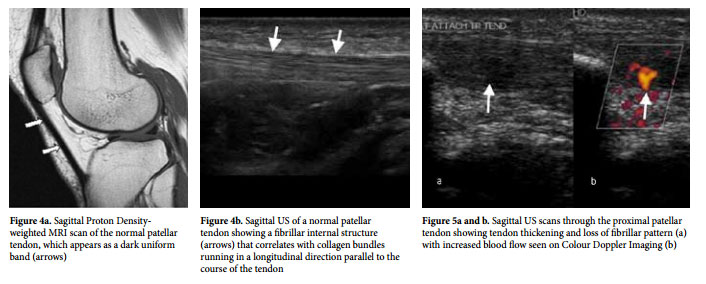
In adolescents, after growth plate closure, injuries at tendon attachment sites are generally referred to tendinopathies; the term tendinopathy refers to a combination of pathologies that include tendinosis (collagen degeneration, fibre disorientation and accumulation of mucoid substance), tendinitis (findings of tendinosis and the presence of inflammatory cells) and paratendinitis (inflammation of the paratenon). Unlike MRI, which shows healthy tendons as homogeneous dark bands in all imaging protocols (Fig 4a), ultrasound is able to distinguish a fibrillar pattern running longitudinally through the tendon that correlates with collagenous fibre bundles (Fig 4b).
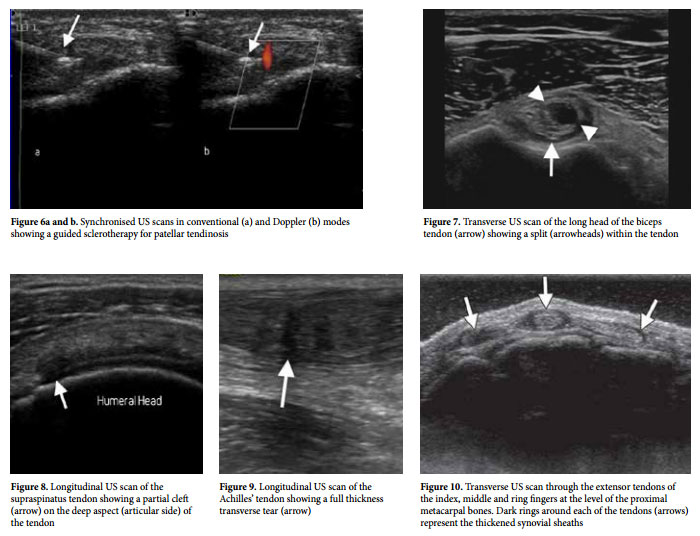
US findings of tendinosis include focal thickening with heterogeneous decreased echogenicity and loss of the normal fibrillar pattern (Fig 5a). Assessment of the area of abnormal texture with Colour Doppler US may show an area of increased blood flow (Fig 5b). Detection of these findings is not only useful for diagnosis of tendinosis but also for guiding treatments. Such treatments may include needling or fenestration, which induces haemorrhage and inflammation, both of which stimulate production of growth factors to promote healing. Platelet Rich Plasma (PRP) infiltration has the same effect. On the other hand, sclerotherapy – which is achieved by injecting a sclerosant such as polidocanol to occlude the vessels (Fig 6) – results in a decrease in inflammatory response. Although the latter is contradictory to other techniques mentioned earlier, which rely on an inflammatory response to induce healing, sclerotherapy has been shown to have positive results particularly in patellar tendinosis, lateral epicondylitis of the elbow and Achilles’ tendinosis.
Continued overuse in the presence of tendinosis can result in progression to a partial or complete tear. Partial tears may be longitudinal or transverse. Longitudinal tears (also called longitudinal splits) course along the length of the tendon and may resemble tendinosis on US. Longitudinal tears are best seen when the tendon is imaged perpendicular to its course (along the short axis) (Fig 7). Transverse tendon tears are best seen when imaged parallel to the course of the tendon. Partial thickness transverse tears may appear as an irregularity along one margin of the tendon or as a partial cleft within the tendon (Fig 8). A full thickness tear will present as a fluid-filled gap in the tendon with retraction of the proximal and distal segments (Fig 9). Dynamic US assessment during muscle contraction may improve visibility of a transverse tendon tear on ultrasound by opening the gap.
Tenosynovitis is an inflammatory reaction of the tendon synovial sheath, which is the most common type of overuse injury and is readily detected with US. It may present alone with pain located over the tendon and accentuated by tendon movements. Tenosynovitis may also present itself in association with tendinosis and tendon tears. US is highly accurate in detecting tenosynovitis (Fig 10) and in guiding treatment with injection of long acting steroids or PRP into the tendon sheath.
In summary, US has become the first line of management for acute soft tissue injuries. It provides immediate and accurate results in a safe and dynamic fashion. Tendon injuries are frequently better seen on US than with more complex imaging such as MRI. US also provides a means to deliver immediate and targeted treatment to decrease convalescence times. Part II of this article will discuss imaging and treatment of ligamentous injury.