The Impact of COVID – 19 on Epilepsy and its Management
Tamara Attard Mallia & Dr Christian Zammit
ABSTRACT
The current coronavirus pandemic (COVID-19) has had a huge impact on our everyday life. This was even more so for certain cohorts of people, like those who suffer from epilepsy. Internationally, patients experienced difficulties in obtaining their anti-epileptic drugs and/or contacting their local pharmacy. Hospitals have been excessively burdened with COVID-19 patients leading to cancelled out-patients’ appointments. Social isolation has increased epileptic injuries requiring emergency treatment. Epilepsy is not a risk factor to develop COVID-19, but the symptoms of one condition may indeed exacerbate those of the other. Remote healthcare by telemedicine provided a valuable means to mitigate the deleterious effect of COVID-19 on epileptic people.
- INTRODUCTION
Epilepsy is a cerebral disorder characterized by recurrent seizures, the characteristics of which depend on the type of epilepsy. Seizures usually present with sensory or motor phenomena and such patients may or may not experience loss of consciousness.1 This condition is the second most common neurological disorder and is prevalent in approximately 0.7-4.6% of the general population and 6-8% of the pediatric population.2 COVID-19, first identified in Wuhan City, China, over time got widely transmitted and became a worldwide pandemic.3 COVID-19 has proved fatal in over 460 local cases and over 5.1 million people worldwide.4 As a result, people had to socially isolate themselves and limit their contact with others so as to prevent further transmission. This left a significant impact on epileptic patients, among others, as their chronic condition could not be managed with the usual protocol.
1.1 ASSOCIATIONS BETWEEN COVID-19 AND EPILEPSY
Initial data obtained by the Center for Disease Control and Prevention (CDC) suggested that epilepsy is a risk factor for COVID-19, but further analysis by the CDC did not establish a direct link between these two conditions.5,6 However, epilepsy possibly increases risks of more severe symptoms of COVID-19 due to side-effects of anti-epileptic drugs (AEDs) that are mainly used to control seizures. AEDs namely, lamotigrine and phenytoin, suppress immunoglobulin levels, hence the patient is immunocompromised and at a higher risk of having complications with COVID-19.7,8
Epilepsy could nonetheless be due to, or associated with, other neurological conditions or congenital abnormalities that could have impaired immunity, rendering such patients susceptible to COVID-19 infections.8 Additional research also hypothesized that COVID-19 may increase the risks of sudden unexpected death in epilepsy (SUDEP), since other viral infectious diseases like human herpes virus-6 (HHV6) seem to do so.9,10 However, no such specific correlations with COVID-19 have yet been made.5
Literature on this subject is being regularly updated and as depicted in figure 1, there are already approximately 159 meaningful articles regarding epilepsy and COVID-19 associations on PubMed.
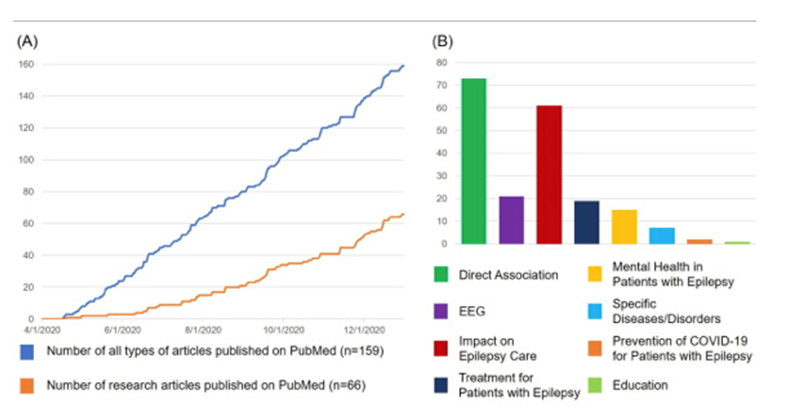
Figure 1: Articles correlating epilepsy and COVID-19 on PubMed. [A] Graph depicting number of articles of all types [blue] and research articles [orange] up to December 1, 2020; [B] classified by topic.6
1.2 EFFECT OF COVID-19 INFECTIONS ON EPILEPTIC PATIENTS
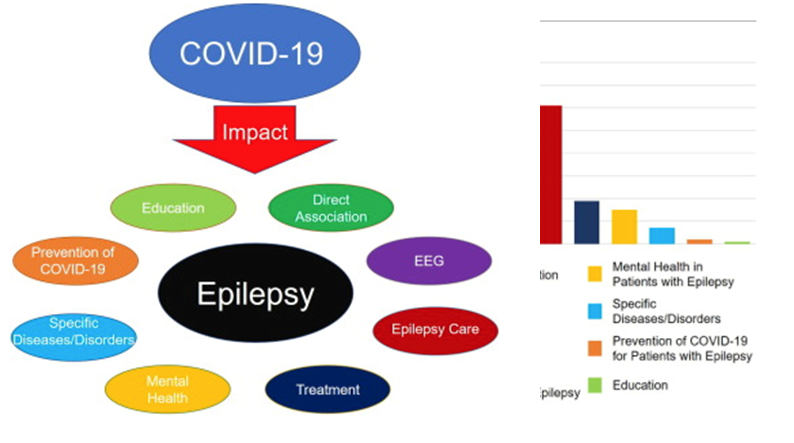
As shown in figure 2, various aspects of epilepsy management were found to be significantly impacted by this pandemic. COVID-19 has been suggested to exacerbate seizure frequency and alter actions of AEDs.
Given that fever may trigger seizure onset, COVID-19 infection and its flu-like symptoms were suggested to exacerbate seizures in epileptic patients mainly due to the inflammatory reaction to the infection.5,11 Moreover, the coronavirus may enter the nervous system via angiotensin-converting enzyme receptor type 2 (ACE2) causing pro-inflammatory cytokines to enter the brain and be further produced by brain neurons namely, astrocytes and microglia. This potentially disrupts the blood brain barrier, increasing the levels of glutamate, gamma-amino butyric acid (GABA) and aspartate which induce seizures.12
Figure 2: Epilepsy-associated factors that have been potentially impacted by COVID-19. These include education, EEG, mental health, and management among others.6
A number of antiviral drugs used to treat COVID-positive patients (like remdesivir) have also been reported to interact with a number of commonly used AEDs (like carbamazepine).13
1.3 EFFECTS OF COVID-19 RESTRICTIONS ON EPILEPTIC PATIENTS
This pandemic has forced people to socially isolate themselves and maintain distance between each other. This has decreased rates of transmission but left serious challenges for everyone.
1.3.1 Prescription Availability
A survey conducted amongst people residing in the UK and suffering from epilepsy by Thorpe et al.14 found that around 13% experienced difficulties in taking medication on time, mainly due to routine changes, and problems with acquiring a prescription. Indicatively, this problem was more prevalent in people with epilepsy (PWE) rather than the caregivers.15 Caregivers might have been too busy taking care of the family due to lockdowns; others also mentioned tele-working that kept them equally busy, as if they were working onsite. The authors also reported that contacting the physician or pharmacists proved difficult and PWE who had their dosage regimen changed during lockdown experienced prescription delays due to unprocessed treatment plans by their physician or pharmacy.14
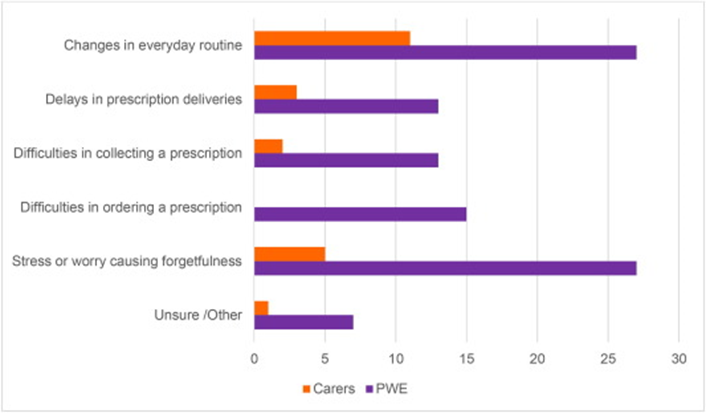
Figure 3: Mentioned reasons for not complying to AED regimen. Graph depicting reasons for not taking AEDs on time by care-givers [orange] and PWE [purple].14
1.3.2 First Aid and Emergency
In the study conducted by Thorpe et al.14 approximately a quarter of the epileptic population was found to have lived socially isolated during the lockdowns; of which 23% made use of safety features namely, seizure alarms or emergency numbers linked with their physician. 15% of socially isolated patients had no one to provide them with first aid and approximately 38% of all PWE reported accidents that needed emergency help in 12 months. 41% of the latter group were living alone when the accident occurred. Indicatively, social isolation has increased the risks of injuries, especially during ictal episodes where patients may lose consciousness.15
1.3.3 Mental Health and Social Isolation
Lockdowns have left PWE isolated and often, helpless. Unfortunately, confinement-related anxiety and depression was significantly reported as shown in figure 4. Sleeping patterns were also significantly impacted due to changes in sleep schedules, longer sleeping hours and thought rumination.16
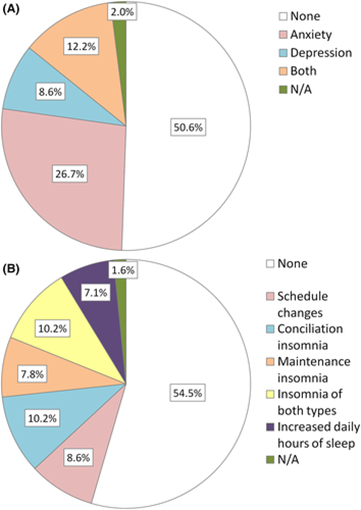
Figure 4: Mental health challenges for PWE due to COVID-19 lockdown. Anxious and depressive symptoms (A) and sleep disturbances (B) in PWE during lockdown.16
Such symptoms tend to reduce seizure control.17 In fact, around 1 in 10 patients reported such changes in seizure control.16 Moreover, recent evidence from southwest China showed psychological distress was at its peak at the time of the initial outbreak of COVID-19. The most prone were mainly drug-resistant epileptic patients as they suffered from more frequent seizures and in keeping with this, they spent longer periods searching for COVID-19 related information on the internet.6,18
Conversely, PWE that had employment-related changes (telework) which led to less work-related stress reported diminished seizure frequency.16 Despite this being a minority, it is interesting that some forms of benefit in certain lifestyles were recorded. However, the negative impacts still seem to prevail and anxiety remained a bigger collateral effect to date.19
- Access to Health Care
Many PWE have struggled with seizure control due to poor medical attention during the pandemic. Cancelled outpatient appointments have proved to be a major cause for concern as such patients may have required changes in their medication. Also, doctors were found to be deployed in COVID-19 wards, rendering them unable to see their patients.20 Conversely, patients that where anxious of the hospital as being highly contagious, cancelled their appointments. In fact, a study published in 2021 reported that 50% of patients with poor seizure control had not contacted their doctor.20 In addition, most patients from the other half that decided toattend outpatients had poorly controlled seizures, indicating that hospital was kept as last resort. Notably, hospital appointments for patients experiencing a first seizure , with a view to make a clinical assessment , were also delayed in approximately 15% of cases.16
1.4 TELEMEDICINE AND VIRTUAL CLINICS
The use of technology to keep physically distant PWE connected with their doctors has been looked into before, but the pandemic provided the perfect opportunity to use this tool.23,24 Telephone calls, instant messaging and SMSs enabled doctors to immediately help their patients despite their location. Video calls were particularly helpful since patients reported that seeing their doctor significantly decreased their anxiety symptoms. 16,25
In keeping with the above, the pandemic has stimulated further epilepsy virtual clinics to be put up in various countries. Patients can still have their appointments from their own home or a digitally equipped place. Some centres in France also offer a remote, epilepsy follow-up device, so as to record the patients’ EEG as well as other physiologic data; these are then electronically sent to the specialist as described in figure 5. These clinics can also serve as potential distributors of AEDs whilst directly sending prescriptions of patients to pharmacies to keep the everything up-to-date.26
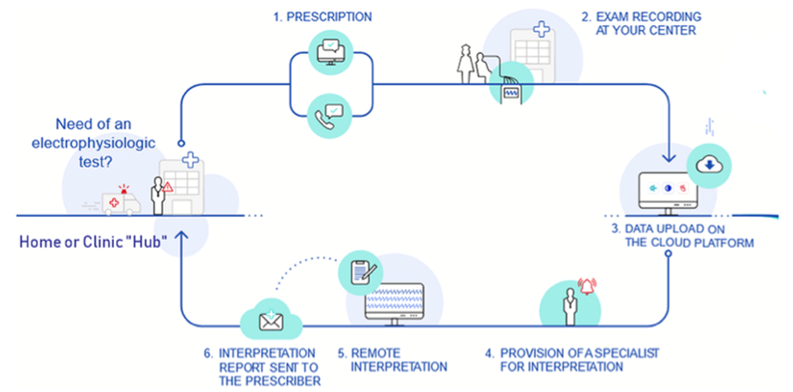
Figure 5: Virtual epilepsy clinic diagnostic journey..27
- CONCLUSION
COVID-19 has left an indelible impact on the provision of healthcare around the world, and this includes the care received by PWE. This is a major cause for concern as doctors and patients have to think on their feet as to how they are to keep contact. Hence, technology and remote healthcare have proven formidable to prevent miscommunication, misdiagnoses or incompliance; decreasing complications and the need to seek urgent care is thus minimized. Proper epilepsy management and education to PWE’s relatives is also crucial as the patient’s household may become the first-responder when a seizure arises.
References
- Sridharan R. Epidemiology of Epilepsy. Curr Sci 2002;82(6):664–70.
- Albuja AC, Murphy PB. Absence Seizure. [Updated 2021 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021.
- World Health Organization. Coronavirus disease (COVID-19) pandemic [Online]. World Health Organization – Europe. 2020. Available from: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov (accessed 19 Apr 2021).
- World Health Organization (WHO). WHO Coronavirus (COVID19) Dashboard [Online]. World Health Organisation. 2021 Available from: https://covid19.who.int/region/euro/country/mt (accessed 18 November 2021).
- Kuroda N. Epilepsy and COVID-19: Associations and important considerations. Epilepsy Behav 2020;108:107122.
- Kuroda N. Epilepsy and COVID-19: Updated evidence and narrative review. Epilepsy Beha 2021;116:107785.
- Godhwani N, Bahna SL. Antiepilepsy drugs and the immune system. Ann Allergy Asthma Immunol 2016;117(6):634–40.
- Epilepsy Foundation. COVID-19 and Epilepsy [Internet]. 2020. Available from: https://www.epilepsy.com/sites/core/files/atoms/files/COVID%20and%20Epilepsy%20051220%20FINAL.pdf (accessed 25 Apr 2021).
- Andersen ML, Tufik S, Colombo AL, et al. Sudden unexpected death in children with epilepsy: the many faces of fungal pathogenicity. Med Hypotheses 2012;79(2):127–8.
- Wang J, Huff K, McMasters R, et al. Sudden unexpected death associated with HHV-6 in an adolescent with tuberous sclerosis. Pediatr Neurol 1999;21(1):488–91.
- Vohora D, Jain S, Tripathi M, et al. COVID-19 and seizures: Is there a link? Epilepsia 2020;61(9):1840–53.
- Nikbakht F, Mohammadkhanizadeh A, Mohammadi E. How does the COVID-19 cause seizure and epilepsy in patients? The potential mechanisms. Mult Scler Relat Disord 2020;46:102535.
- Russo E, Iannone L. Clinically relevant Drug-Drug interaction between AEDs and medications used in the treatment of COVID-19 patients [Internet]. Italian League Against Epilepsy 2020. Available from: https://www.lice.it/pdf/Antiepileptic_drugs_interactions_in_COVID-19.pdf (accessed 25 Apr 2021).
- Thorpe J, Ashby S, Hallab A, et al. Evaluating risk to people with epilepsy during the COVID-19 pandemic: Preliminary findings from the COV-E study. Epilepsy Behav 2020;115:107658.
- Van Hees S, Siewe Fodjo JN, Wijtvliet V, et al. Access to healthcare and prevalence of anxiety and depression in persons with epilepsy during the COVID-19 pandemic: A multicountry online survey. Epilepsy Behav 2020;112:107350.
- Fonseca E, Quintana M, Lallana S, et al. Epilepsy in time of COVID-19: A survey-based study. Acta Neurol Scand 2020;142(6):545–54.
- Moots PL, Maciunas RJ, Eisert DR, et al. The course of seizure disorders in patients with malignant gliomas. Arch Neurol 1995;52(7):717–24.
- Hao X, Zhou D, Li Z, et al. Severe psychological distress among patients with epilepsy during the COVID-19 outbreak in southwest China. Epilepsia 2020;61(6):1166–73.
- Miller WR, Von Gaudecker J, Tanner A, et al. Epilepsy self-management during a pandemic: Experiences of people with epilepsy. Epilepsy Behav 2020;111:107238.
- Rosengard JL, Donato J, Ferastraoaru V, et al. Seizure control, stress, and access to care during the COVID-19 pandemic in New York City: The patient perspective. Epilepsia 2021;62(1):41–50.
- Davico C, Marcotulli D, Lux C, et al. Where have the children with epilepsy gone? An observational study of seizure-related accesses to emergency department at the time of COVID-19. Seizure 2020;83:38–40.
- Yang C, Hao Z, Yu D, et al. The prevalence rates of medication adherence and factors influencing adherence to antiepileptic drugs in children with epilepsy: A systematic review and meta analysis. Epilepsy Res 2018;142:88–99.
- Chi N-C, Demiris G. A systematic review of telehealth tools and interventions to support family caregivers. J Telemed Telecare 2015;21(1):37–44.
- Tschamper MK, Jakobsen R. Parents’ experiences of videoconference as a tool for multidisciplinary information exchange for children with epilepsy and disability. J Clin Nurs 2019;28(9–10):1506–16.
- Brigo F, Bonavita S, Leocani L, et al. Telemedicine and the challenge of epilepsy management at the time of COVID-19 pandemic. Epilepsy Behav 2020;110:107164.
- Lavin B, Dormond C, Scantlebury MH, et al. Bridging the healthcare gap: Building the case for epilepsy virtual clinics in the current healthcare environment. Epilepsy Behav 2020;111:107262.
- Serenity Medical Services. Virtual Clinic [Online]. Available from: https://www.bioserenity.com (accessed 9 Jul 2021).

