Smoking in the 21st century
Dr Moses Camilleri
Introduction
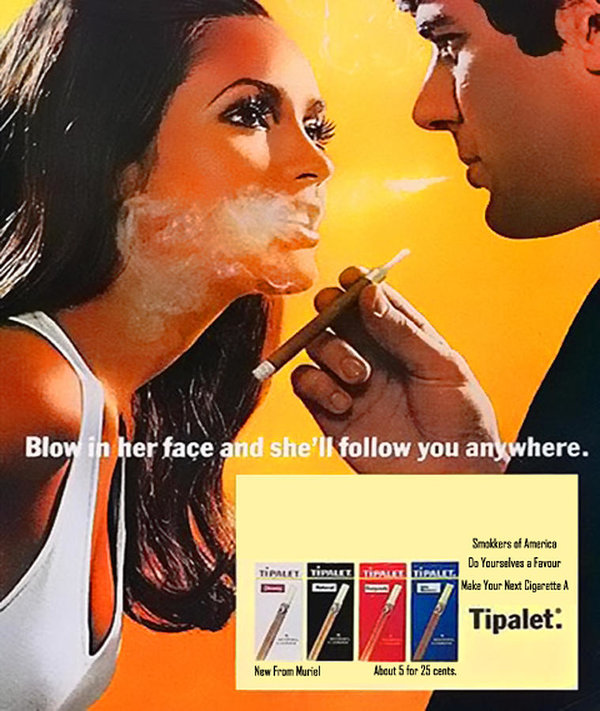
Jean Nicot de Villemain (1530 – 1600) was a French diplomat who became famous for introducing tobacco to France. Little could he imagine the immense upheaval he would bring to future generations. Up until the early 1900’s, smoking cigarettes was made to look glamorous and even had health benefits attributed to it.
However, the link between smoking and respiratory diseases had been established back in the early 1900s in studies by European and American doctors but this remained a taboo up until the 1950s.1 As time went by, the evidence linking smoking as the cause of disease continued to accumulate and, what was a controversy in the 1960s and 1970s, turned into outright condemnation in the 1980s. Although the medical profession had more knowledge about the harm caused by smoking, the general public was less informed because cigarette manufacturers were doing their best to cast doubt on how true these “allegations” were. Mass legal action instituted in the 1990s led to the Master Settlement Agreement in 1998 with US courts condemning major US cigarette companies to pay huge sums of money to the US government over a period of 25 years to compensate for some of the damage and expenses incurred in caring for the millions of people suffering ill health directly caused by smoking over the years.2
Over the past couple of decades, regulations to control tobacco use have fallen short of outright prohibition. With current knowledge of the harm caused by smoking, this would be a sensible thing to do. But experience has taught us that prohibition, while reducing use of a substance in the general population, does not really stop those who are intent on using the prohibited substance from doing so.3,4 Legislation to control tobacco use aims at reducing harm to smokers and protect non-smokers from exposure to exhaled secondary smoke. It is surprising that, the Manufacture, Presentation and Sale of Tobacco and Related Products Regulations (S.L. 315.10), enacted under the Tobacco (Smoking Control) Act (Cap. 315) , actually identifies the addictive properties of nicotine and defines “addictiveness as the pharmacological potential of a substance to cause addiction”, which is described as “a state which affects an individual’s ability to control his or her behaviour, typically by instilling a reward or a relief from withdrawal symptoms, or both.” By 2016, Maltese legislation with regards to smoking control was updated to reflect EU law. The law specifies measures to control not only concentration of nicotine in cigarettes but, probably of more importance, the law describes which cancerogenic substances are allowed. Surprisingly, the law permits use of chemicals that are known to make the smoker sick and possibly sick enough to die! Keeping up with the times, the same legislation S.L. 315.10 confirms that smokeless tobacco is illegal in Malta and also defines and describes electronic cigarettes.
This brings me to the subject of smoking other than conventional cigarettes. Probably most people assume that smoking is the act of putting a tobacco-filled cigarette to one’s mouth and lighting it up. The process of burning tobacco reaches a temperature as high as 650°C where chemicals that are known to be cancerogenic tend to be more harmful to the lung tissue of the smoker. However, tobacco can also be smoked without burning (combusted or heat-not-burn/HNB) by using a battery-operated device to power a heating element, which when in contact with tobacco, heats rather than burns the tobacco. This mode of nicotine delivery system (the polite way to refer to smoking) heats up tobacco to a temperature of 300 to 350°C, generating a vapour that is inhaled by the smoker. At the lower temperature, the cancerogenic chemicals in tobacco are thought to be less harmful to the smoker.
The latest fad in smoking is the use of what are known as electronic cigarettes. Like combusted cigarettes, electronic cigarettes are battery-operated but instead of heating tobacco, a solution is heated to generate a vapour inhaled by the smoker. This is referred to as vaping.

Appearing on the market towards the end of the 20th century, the first electronic cigarettes were patented in 2003 and appeared in China in 2004, in Europe two years later and the US in 2007. The prevalence of electronic cigarettes in the general population is 3.5 to 5.5%, but prevalence studies indicate it is a fad that has mostly engaged young people and adolescents. Some US studies indicate rates as high as 46% in this cohort. Most people who use electronic cigarettes also smoke conventional cigarettes at some stage during their smoking career. Studies indicate that electronic cigarettes might serve as a gateway for the use of conventional cigarettes. Among factors contributing to the prevalence of e-cigarette use cited by young people is the exposure to robust advertising campaigns, the ability to customize devices, flavours, nicotine content, peer use, enjoyment, and curiosity.5,6 This prompted US authorities earlier this year to limit the flavours that could be included in electronic solutions (e-solutions, e-liquid, or e-juice). This was done to reduce the appeal that smoking flavoured e-cigarettes might have to younger users.

A major influence contributing significantly to favourably change the perception towards e-cigarettes in the general population but also in the medical community, was a 2014 study, which sought to estimate the harm of nicotine-containing products through modelling techniques. It concluded that conventional smoking was 20 times more harmful than vaping e-cigarettes.7 The UK Public Health took this up and started advertising the use of e-cigarettes, which it said were “at least 95% less harmful than cigarettes”. This study has been contested with claims that advances in technology allows bigger power generation resulting in more vapour production and exposure of the user and bystanders to more, possibly harmful chemicals, and the ever increasing variety of flavours made up of chemicals that might be considered safe to eat but with as yet unknown consequences when inhaled. Another advancement has been the development of protonated nicotine which allows higher concentrations of nicotine to be inhaled without causing throat irritation, with the consequence of higher addiction to nicotine.8
With the current understanding, should smokers be encouraged to change to vaping to improve their health? Unfortunately, there are different thoughts on this. A study in 2017 followed vapers who smoked e-cigarettes exclusively for 3.5 years and found no detriment to their health, even when investigated extensively. The study does highlight that 3.5 years is a short period of time to follow up for possible harm.9 The World Health Organization remains uncommitted as to whether e-cigarettes should be advocated, neither as a means of smoking cessation nor as a means of harm reduction.10

As to second-hand smoke exposure, studies comparing vapour generated by e-cigarettes and that by conventional ones, indicate that the latter generate more particles and stay around for longer periods of time.11 Yet it is well known that the belief that e-cigarettes generate only a water vapour is certainly a misconception. Studies indicate particles in e-cigarette generated vapour to be cancerogenic, harmful to the unborn and a source of indoor pollution.12
Of concern with the use of e-cigarettes has been the observation of a newly identified lung disease referred to as e-cigarette and vapour product use-associated lung disease (EVALI). First noticed in early 2017 in the US, some cases have also been reported in Europe. Patients complain of a cough, chest pain and shortness of breath. While some patients improve with no need for hospital care, others are not so lucky. By mid-January 2020, 2,668 hospitalized EVALI cases were reported in the US and nearly half the patients required intensive care to treat respiratory failure. Sixty died. Most patients were younger than 35 years old. While the exact cause of EVALI is still being investigated, it is well documented that all patients presenting with this condition had been vaping in the three months before getting sick. It has been confirmed that this condition is not an infective but rather an inflammatory process that causes lung injury. Of interest is the presence of tetrahydrocannabinol (THC) which is the active ingredient in marijuana (cannabis), in up to 80% of e-solutions that had been used by patients presenting with this condition. In up to half of the implicated e-solutions, another component found was vitamin E acetate (VEA). This is an additive that started being used in e-solutions as a cutting agent to thicken the solution. While VEA is considered safe to eat, it seems that its safety profile significantly changes when inhaled as a vapour. In such a scenario the Food and Drug Administration (FDA) in the US could only strongly advise e-cigarette users to avoid use of vaping products that were spiked with THC and to buy e-solutions only from reliable sources. It seems vapers are heeding this advice as new cases of EVALI have dropped since October 2019.13,14
A new challenge with the ever-increasing number of vapers, is the further risk that comes with spiking of e-solutions with dangerous drugs of abuse.
Of concern is the presence of psychedelic substances and opioids such as fentanyl (at least 50 times stronger than heroin) in e-solutions. While not yet a widespread problem, it is envisaged that this new mode of drug administration could present itself as a new challenge to services caring for people who use drugs.14 It is important that users of e-cigarettes are made aware of the dangers involved when buying e-solutions from sources that are not certified as required by The Manufacture, Presentation and Sale of Tobacco and Related Products Regulations (S.L. 315.10), enacted under the Tobacco (Smoking Control) Act (Cap. 315). The aforementioned Regulations stipulate that electronic cigarettes are subject to a number of safeguards (e.g. maximum concentration of nicotine of 20 mg/ml, maximum single use cartridge size of 2 ml) and requirements (e.g. notification to the competent authority prior to placing on the market, reporting of ingredients, inclusion of an information leaflet, and specific rules on advertising).
Vapers who intentionally want to use drugs of abuse administered by utilizing an e-cigarette, should be aware of the dangers involved and ensure safer use by following harm reduction guidelines such as starting off with lower doses, not mixing drugs and avoid as much as possible use of such substances when on their own. Help to address one’s drug use is available. Sedqa may be contacted on helpline 179, 24 hours a day and 2388 5110 during office hours.
References
- Proctor R. The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll. Tobacco Control 2012; 21(2):87-91.
- Sloan F. Impacts of the Master Settlement Agreement on the tobacco industry. Tobacco Control 2004;13(4):356-361.
- Hall W. What are the policy lessons of National Alcohol Prohibition in the United States, 1920-1933? Addiction 2010;105(7):1164-1173.
- Courtwright D. Commentary on Hall (2010): The difference a word makes – a short history of ‘prohibition’. Addiction 2010;105(7):1174-1175.
- Hiler M, Spindle T, Dick D, et al. Reasons for Transition From Electronic Cigarette Use to Cigarette Smoking Among Young Adult College Students. Journal of Adolescent Health 2020;66(1):56-63.
- Kintz N, Liu M, Chou C, et al. Risk factors associated with subsequent initiation of cigarettes and e-cigarettes in adolescence: A structural equation modeling approach. Drug and Alcohol Dependence 2020;207:107676.
- Nutt D, Phillips L, Balfour D, et al. Estimating the Harms of Nicotine-Containing Products Using the MCDA Approach. European Addiction Research 2014; 20(5):218-225.
- Sood A, Kesic M, Hernandez M. Electronic cigarettes: One size does not fit all. Journal of Allergy and Clinical Immunology 2018; 141(6):1973-1982.
- Polosa R, Cibella F, Caponnetto P, et al. Health impact of E-cigarettes: a prospective 3.5-year study of regular daily users who have never smoked. Sci Rep 2017;7:
- WHO: E-cigarettes, Questions & Answers, 29 January 2020. Accessed 17 September 2020. Available at https://www.who.int/westernpacific/news/q-a-detail/e-cigarettes-how-risky-are-they
- Protano C. Second-hand smoke exposure generated by new electronic devices (IQOS and e-cigs) and traditional cigarettes. Ann Ig 2016;28:109-112.
- Marcham C, Springston J. Electronic cigarettes in the indoor environment. Reviews on Environmental Health 2019;34(2):105-124.
- EU Early Warning System Briefing Update – Outbreak of serious lung injury among people who use e‐cigarette products (vaping) – Multiple States, United States, 2019 (ongoing); RCS ID: EU‐EWS‐RCS‐BR‐2019‐0004‐U2 – EMCDDA – December 2019.
- Werner A, Koumans E, Chatham-Stephens K, et al. Hospitalizations and Deaths Associated with EVALI. New England Journal of Medicine 2020; 382(17):1589-1598.

