Skin Microbiota and Body Malodour
DR Etienne Grech, Dr Georgiana Farrugia Bonnici, Dr Martina Hohman
ABSTRACT
Chronic body malodours are often considered to be universal triggers of distress for many patients. Various human body malodours relate to the bacterial transformation of compounds conveyed by sweat on the skin surfaces and axillae. There is skin microbiome variation between individuals which typically results in a change in one’s sweat constitution and ultimately influences the final odour produced. Body malodour may be managed through good personal hygiene, the use of antiperspirants, deodorants, zinc emulsions, antifungals, glycopyrronium tosylate, triclosan body soaps and povidone-iodine. Moreover, certain lifestyle modifications, the use of oral probiotics and prebiotics, along with more invasive medical and surgical procedures, such as axillary laser therapy, iontophoresis, Botulinum toxin type A, suction-curettage, elliptical axillary skin excision as well as transthoracic sympathectomy may also result in body malodour suppression. In this article, the relationship between bacterial skin commensals and body malodour will be discussed.
INTRODUCTION
Chronic body malodours are often considered to be universal triggers of distress for many patients.1 They may result in significant negative psychological, social and sexual outcomes, such as low self-esteem, anxiety, impaired quality of life, social exclusion as well as decreased intimacy.2 There are various odours which are emitted by the human body, including but not limited to the oral, reproductive, dermatological, urinary, apocrine and endocrine systems.2 Phages, archaea, mites, viruses, fungi and bacteria may all form part of the skin microbiome, some of which have been documented to affect various skin properties, immune responses, pathogen growth and wound healing.3-5 Human body malodours relating to the bacterial transformation of compounds conveyed by sweat in the skin surfaces and axillae, will be discussed in greater detail.
THE ANATOMY AND PHYSIOLOGY OF HUMAN SKIN AND SWEAT PRODUCTION
The largest organ in the human body is the skin, which has a number of important functions.3 This includes its ability to act as a physical barrier and offer protection against insults from the external environment.3 The skin also supports a diverse microbiota, including bacteria. Although bacteria are primarily associated with infection, one must bear in mind that not all bacteria are harmful to the human body. On the contrary, certain bacteria are beneficial to humans. This may be appreciated by considering the variety of bacteria that are known to colonise the human skin, which ultimately may contribute to protecting humans from pathogens.4,5
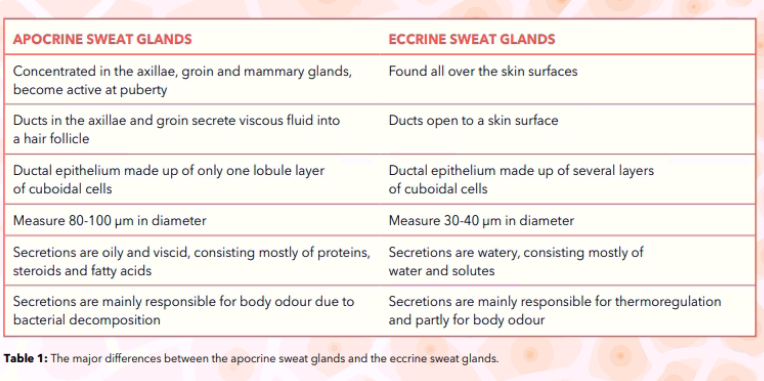
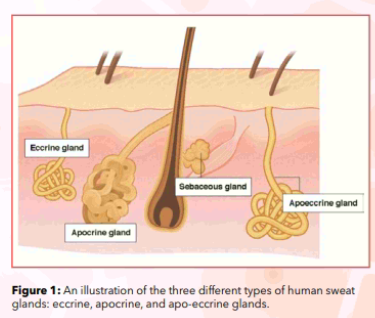
The skin is divided into two parts; the superficial epidermis, consisting of a stratified epithelium, and the deeper dermis, which is made up of a dense connective tissue containing blood vessels, lymphatic vessels and nerves.6 The dermis is also connected to the deep fascia by the subcutaneous tissue. The skin appendages are made up of the nails, hair follicles, sebaceous glands and sweat glands.6 Sebaceous glands pour sebum onto the hair shafts, whilst sweat glands are long, spiral, tubular glands which are distributed over several body surfaces, except for the margins of the lips, the nail beds, the glans penis and the clitoris.6 There are three types of human sweat glands. The eccrine sweat glands are mainly responsible for thermoregulation, which is carried out by secreting water-rich sweat over various body surfaces. Contrastingly, the apocrine sweat glands are restricted to the axillae, mammary glands and groin, which initially produce an odourless, oily, opaque secretion which then gains its characteristic odour from bacterial decomposition.6 It is known that the axillary anatomy provides a favourable environment for bacteria to flourish.7 The third type, the apo-eccrine glands, are also identified in the same areas of the apocrine glands. Similarly, the apo-eccrine glands also secrete watery substances.6 The various differences between the two major types of sweat glands, the apocrine glands and the eccrine glands, are outlined in Table 1 and Figure 1.
On average, humans have two to four million sweat glands. It is also estimated that in adults, the maximum sweat rate is up to 10 to 14 litres daily.6 The components of sweat are primarily water, with small amounts of solutes and trace minerals, such as sodium, potassium, calcium, lactate, urea, magnesium, zinc, copper, iron, chromium, nickel and lead.6 Sweat has a moderately acidic to neutral pH, typically ranging between 4.5 and 7.6 Certain chemical compounds are also found in sweat, such as thioalcohols, carboxylic acids, fatty acids, ketones, ammonia, sulphides, aldehydes, esters, androstene steroids as well as hydrocarbons.7-11 Even though human sweat is initially odourless, the enzymatic action of resident skin bacteria then transforms these odourless precursors to volatile chemical compounds. Over time, a distinct body malodour is produced.7,9-11
There is skin microbiome variation between individuals which may be attributed to a number of different factors. These include the living environment, the working environment, lifestyle including diet, hygiene, ethnicity, gender, the health status of the host, age, as well as antibiotic use, cosmetics and textiles.3,12 This variation in skin microbiota typically results in a change in one’s sweat constitution, and ultimately influences the final odour produced.2,7 Interestingly, it is thought that humans may have been given an adaptive evolutionary advantage due to the specific biosynthesis and secretion of odourants.7 Various kinds of societal information and messages in mammals are thought to be sent via these volatile odours.8 Moreover, this may have an impact on mating selection as humans are highly sensitive to odourants.7 Furthermore, it has been proposed that both odour-producing bacteria and human beings have evolved in conjunction with one another.8
BACTERIAL SKIN COMMENSALS AND OTHER CAUSES OF BODY MALODOUR
The commonest bacteria that have been previously identified on the skin include Gram positive bacteria, such as Staphylococci, Streptococci, Micrococci, Cutibacteria, Corynebacteria, Anaerococci and the Peptoniphilus species, as well as Gram negative bacteria such as Acinetobacter species.5,10,12 In particular, Corynebacteria produce carboxylic acids and androgen steroids which contribute to a pungent axillary odour.7,9,11 Contrastingly, an acidic and sulphur-like odour is produced by Staphylococci through the synthesis of short-chain fatty acids and thio-alcohols.7,9,11 As has been previously discussed, the composition of body odours is mostly determined by genetics and ethnicity.9,12,13 However, it may be influenced through other factors such as age, temperature, diseases, skin pH, physiological and emotional states, diet and bacterial metabolic activity in the gut, as well as personal hygiene.2,5,9 Moreover, it is known that body odours are also discriminable by gender. Male axillary odours tend to be more intense than female axillary odours.9,13 This could result from the fact that men have Coryneform-dominant microflora.9 On the other hand, the production of androstenes is sexually dimorphic. Women tend to secrete lesser quantities of androstenone than men, whilst estratetraenol is mainly produced during pregnancy.13 Furthermore, body odour is also related to intestinal, thyroid, cardiac, liver and renal function.2,7,11 In fact, the body odour of sick individuals is more aversive than that of healthy persons.9 Human malodour may be associated with conditions such as obesity, menopause, anxiety, toxin ingestion, bromhidrosis, halitosis, hyperhidrosis, phenylketonuria, methionine malabsorption syndrome, hypermethioninaemia, trimethylaminuria, maple syrup disease, liver failure, end-stage renal failure, bacterial vaginosis, urinary incontinence and diabetic ketoacidosis.2,6,7
MANAGEMENT OF SKIN MALODOUR
The first step in reducing body malodour is maintaining good personal hygiene, which includes daily bathing with low pH soaps as well as the regular washing of clothes and linen.14 Shaving, waxing, or axillary laser hair removal may also reduce body malodour by decreasing the amounts of bacterial skin microflora.14 Most anti-perspirants contain aluminium salts, which diminish perspiration by blocking the sweat gland excretory ducts, hence reducing bacterial proliferation.14 The use of an anti-perspirant at night will block excretory channels by day-time. Unlike antiperspirants, deodorants mask body malodours with perfume. Zinc emulsions applied to the under-arms, groins, and various other body folds absorb malodours.14 Moreover, antifungal creams such as clotrimazole, miconazole and ketoconazole have also been shown to reduce body malodour, especially if preceded by dilute hydrogen peroxide cleansing.14 The application of topical 2.4% glycopyrronium tosylate on a pre-moistened cloth to the axillae decreases sweat.15,16 Triclosan-based body soaps have been used for decades, due to the lack of resistance of malodour-forming bacteria.2 In addition, the antibacterial compound povidone-iodine also reduces the malodorous scent which is typically created by androstenone in sweat.2
Some dietary substrates which are metabolised by bacteria in the stomach and intestines may eventually end up in body fluids, including sweat, thereby causing body malodour.2 In such cases, one needs to ensure dietary modifications, as well as the avoidance of particular foods, such as garlic, curry, onions and alcohol.2 Oral probiotics and prebiotics may also help in favourably altering the gut bacterial flora.2 Frequent bowel movements will speed up the passage time and hence, decrease unwanted gut bacterial metabolism and metabolite absorption. Furthermore, increasing water consumption also increases the urinary excretion of metabolites, which in turn decreases body malodour.2
More invasive treatment may be undertaken to reduce axillary or palmar hyperhidrosis or bromhidrosis, depending on the severity of each particular case. Treatment with an 800-nm diode or a 1064-nm Nd-Yag lasers may permanently destroy axillary sweat glands by heating them, without injuring the surrounding tissues.14 Such treatment usually takes less than one hour.14 Moreover, microwave treatment may fibrose both the eccrine and the apocrine glands in order to alleviate axillary hyperhidrosis. Such treatment is best conducted with tumescent anaesthesia and microneedle radiofrequency.14,16 Nevertheless, such methods require further research. Iontophoresis, on the other hand, involves a complicated mechanism of ion transport via the skin that blocks the sympathetic innervation of sweat glands in the axillae, the palms of the hands or feet. Iontophoresis employs a local electric current to attract tap water or anti-cholinergic drug ions into the axillary subdermal tissues.16,17
Botulinum toxin type A may also be injected in various parts of the axillae to reduce body malodour, by blocking the sympathetic innervation that releases sweat. This method is safe and efficient, with its effect typically lasting around 6 to 8 months.14,15,17 Another minimally invasive procedure for treating axillary hyperhidrosis, known as suction-curettage partly takes out the deep skin layer that contains sweat glands.18 Malodour may also be significantly reduced by an elliptical axillary skin excision.16,17 Axillary and palmar hyperhidrosis can also be treated through the removal or disconnection of the T2-T4 thoracic ganglia via endoscopic, transthoracic sympathectomy.16-18 However, 8 • thesynapse.net Vol 21 2022 • Issue 02 due to the significant risks involved, such treatment is not recommended as first-line.
CONCLUSION
Medical science is still evolving when it comes to developing new targeted therapies for body malodour. This can be seen in the potential niche that is currently lacking in the development of therapy targeted towards the skin microbiota.5 An advanced understanding of the molecular, biochemical and bacterial pathways involved in body malodour may encourage the development of new microbial therapeutics for various skin conditions which would ultimately benefit many individuals.19 An example of which could possibly include therapy geared towards the inhibition of peptide transporters involved in thioalcohol recognition and transport.8 Even though several theories and hypotheses have been put forward, there is a need for more research and evidence-based medicine in this field.
ACKNOWLEDGEMENTS, COMPETING INTERESTS, FUNDING STATEMENTS
None.
REFERENCES
1. Zakrzewska MZ, Liuzza MT, Lindholm T, et al. An Overprotective Nose? Implicit Bias Is Positively Related to Individual Differences in Body Odor Disgust Sensitivity. Frontiers in psychology 2020; 11:301.
2. Mogilnicka I, Bogucki P, Ufnal M. Microbiota and Malodor – Etiology and Management. Int J Mol Sci 2020; 21(8):2886.
3. Skowron K, Bauza-Kaszewska J, Kraszewska Z, et al. Human Skin Microbiome: Impact of Intrinsic and Extrinsic Factors on Skin Microbiota. Microorganisms 2021; 9(3):543.
4. Byrd L, Belkaid Y, Segre J. The human skin microbiome. Nature Reviews Microbiology 2018; 16:143-155.
5. Timm CM, Loomis K, Stone W, et al. Isolation and characterization of diverse microbial representatives from the human skin microbiome. Microbiome 2020; 8(1):58.
6. Wilke K, Martin A, Terstegen L, et al. A short history of sweat gland biology. Int J Cosmet Sci. 2017; 29(3):169-79.
7. Natsch A, Emter R. The specific biochemistry of human axilla odour formation viewed in an evolutionary context. Phil. Trans. R. Soc. B Sci 2020; 375: 20190269.
8. Minhas GS, Bawdon D, Herman R, et al. Structural basis of malodour precursor transport in the human axilla. Elife 2018;7:e34995.
9. Ferdenzi C, Richard Ortegón S, Delplanque S, et al. Interdisciplinary challenges for elucidating human olfactory attractiveness. Philos Trans R Soc Lond B Biol Sci 2020;375(1800):20190268.
10. Furukawa S, Sekine Y, Kimura K, et al. Simultaneous and multi point measurement of ammonia emanating from human skin surface for the estimation of whole body dermal emission rate. J Chromatogr B Analyt Technol Biomed Life Sci. 2017; 1053:60-64.
11. Rudden, M, Herman R, Rose M, et al. The molecular basis of thioalcohol production in human body odour. Sci Rep 2020; 10(1):12500.
12. Li M, Budding AE, Van der Lugt-Degen M, et al. The influence of age, gender and race/ethnicity on the composition of the human axillary microbiome. Int J Cosmet Sci 2019; 41(4):371-377
13. Damon F, Mezrai N, Magnier L, et al. Olfaction in the Multisensory Processing of Faces: A Narrative Review of the Influence of Human Body Odors. Frontiers in Psychology 2021; 12:750944.
14. Grabell DA, Hebert AA. Current and Emerging Medical Therapies for Primary Hyperhidrosis. Dermatol Ther (Heidelb) 2017; 7(1):25-36.
15. Michael E Stuart, Sheri A Strite, Kristin Khalaf Gillard. A systematic evidence-based review of treatments for primary hyperhidrosis. J Drug Assess 2021; 10(1):35–50.
16. Liu V, Farshchian M, Potts GA. Management of Primary Focal Hyperhidrosis: An Algorithmic Approach. J Drugs Dermatol 2021; 20(5):523-528.
17. Brackenrich J, Fagg C. Hyperhidrosis. StatPearls [Internet] 2021. Accessed on December 20, 2021.
18. Karmota AG, Aboollo MF, Hafez BA, et al. Prospective randomized study comparing Video assisted thoracoscopic surgery (VATS) resection versus cautery for treatment of primary hyperhidrosis. Journal of the Egyptian Society of Cardio-Thoracic Surgery 2018; 26(4):318-323.
19. Casterline BW, Paller AS. Early development of the skin microbiome: therapeutic opportunities. Pediatr Res
2021; 90(4):731-737.

