Management of Incidentally Noted Adnexal Cystic Lesions
Dr Pierre Vassallo
Adnexal cysts are a very common incidental finding on all cross-sectional imaging modalities, specifically ultrasound (US), computed tomography (CT) and magnetic resonance imaging (MRI). They may cause unnecessary concern and lead to unnecessary imaging and possibly also to surgical interventions. In one study, 15% of patients undergoing routine pelvic US were referred for follow-up of an incidentally noted adnexal cyst.1 In another study that evaluated almost 11,600 women undergoing surgery for adnexal masses, 21% were benign serous cysts and 15% were functional cysts;2 surgery would have been avoided in most of these cases had a standardised clinical/imaging-based classification been employed.
A large majority of adnexal cysts are benign and can be managed with imaging or no follow-up. Management decisions are based on the patient’s age and pre/post-menopausal status, and on imaging features detected on US.
Classification of Adnexal Cysts
There are three main consensus articles published between 2019 and 2020 that can be combined to classify cystic lesions based on clinical and imaging findings;3-5 these documents recommend further management based on lesion classification. In spite of some size differences between the three documents, a combined classification has been recommended and may be applied in clinical practice for patients who are not pregnant and who have an average risk for ovarian cancer.6 Average risk is a rather vague classification, but it usually refers to those women who have no genetic predisposing conditions and no personal or family history of cancer.
The Society of Radiologists in Ultrasound (SRU) (3) recommends that premenopausal 5-10cm simple cysts are optimally re-evaluated after 6-12 months, whereas the Ovarian-Adnexal Imaging-Reporting-Data System (O-RADS)4 advises that they are re-evaluated after 8-12 weeks. SRU advises short-interval follow-ups (6-12 weeks), or an MRI when an adnexal cyst of any size regardless of menopausal status is not adequately visualised with US, whereas the American College of Radiology Incidental Findings Committee (ACR-IFC)5 recommends that a simple-appearing cyst with limited assessment at CT or MRI does not require further imaging when under 5cm in a pre-menopausal patient or under 3cm in a post-menopausal patient.
It is difficult to implement recommendations from all three aforementioned sources in clinical practice. The mission of the radiologist who detects an adnexal lesion is to classify the lesion according to the following four categories:7
- Very likely non-neoplastic: no further follow-up required;
- Most likely benign even if neoplastic: imaging follow-up required;
- Cannot be confirmed benign but low likelihood of malignancy: further cross-sectional imaging and gynaecologist consultation;
- Moderate-to-high likelihood of malignancy; further cross-sectional imaging and surgical/oncologic intervention.
A unilocular cyst with thin smooth walls containing simple fluid and no solid or vascular components is almost always benign; such lesions are called simple adnexal cysts (Fig 1). Such a lesion, if it is smaller than 5cm in a pre-menopausal woman or smaller than 3cm in a post-menopausal woman, is characterised as very likely non-neoplastic, and no further imaging or follow-up is required.
Larger unilocular cysts (>5cm in pre-menopausal and >3cm in post-menopausal women) that exhibit thin walls and contain no solid or vascular components should be classified as most likely benign even if neoplastic. Such lesions require imaging follow-up with transvaginal US being the imaging modality of choice (Fig 2).
Cystic lesions that show solid components, irrespective of size, should be classified as having a low likelihood of malignancy, but one cannot exclude it. While many of these are benign, the possibility of malignancy mandates further imaging and in most cases surgical intervention (Fig 3).
Cystic lesions showing large solid and hypervascular components particularly in the presence of ascites should be considered as having moderate-to-high likelihood of malignancy irrespective of menopausal state (Fig 4).
Any lesions that fall within categories b and c listed above should be followed up by the imaging radiologist; this will benefit the patient through detection of any changes that alter the lesion’s category, even though this may be rare. In addition, it is beneficial to the radiologist’s personal education as it will improve his/her ability to characterise such lesions. Lesions showing features that suggest a specific diagnosis such as hemorrhagic cysts, hydrosalpinges, peritoneal inclusion cysts, endometriomas, and dermoids may change on follow-up scans and require a revised diagnosis.
Conclusion
Based on a large volume of imaging research studies, we now know that a simple adnexal cyst does not significantly increase a woman’s likelihood of ovarian malignancy regardless of menopausal status. Considerable progress has been made over the past 50 years through advances in diagnostic imaging from the time when all palpable postmenopausal ovaries went to surgery. Simple cysts measuring <5cm in pre-menopausal and <3cm in post-menopausal women do not require further follow-up. Larger lesions and those showing complex features require further imaging, consultation and/or surgical intervention based on the criteria described above.
Figure Legends:
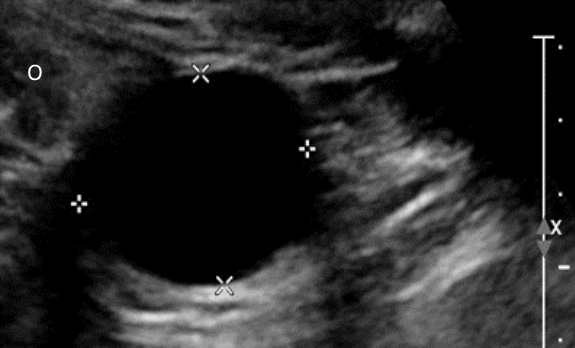
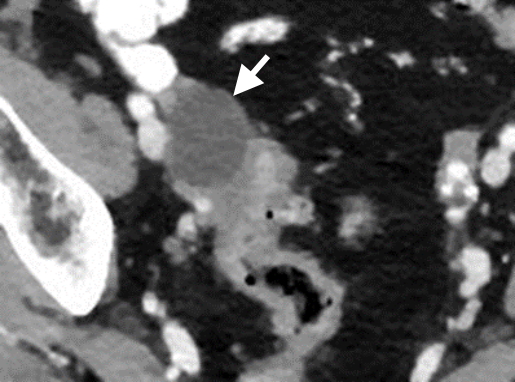
Figure 1.a. Transvaginal US image in a post-menopausal woman showing a 3cm simple cyst (between callipers) with thin walls and no internal structure. Ovary (O). b. CT scan image showing an incidental 3.5cm cyst (arrow) in a post-menopausal woman that had not changed from a CT scan taken 5 years earlier.
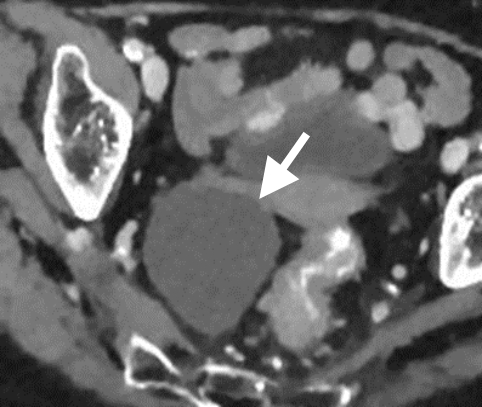
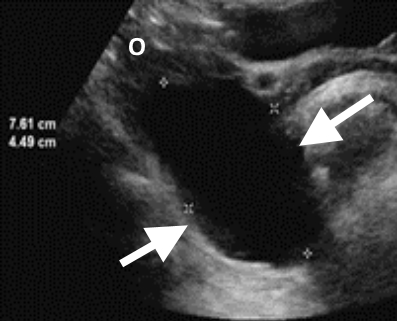
Figure 2.a. Incidentally noted 7cm cyst (arrow) on a CT scan in a post-menopausal woman. b. US follow-up performed after 12 weeks confirms the simple nature of the cyst with no change in size. The lesion was excised at the patient’s request. Histological analysis confirmed a cystadenoma, which is a benign tumor.
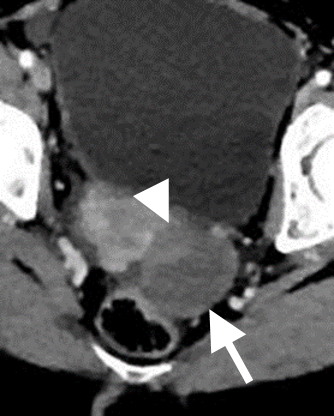
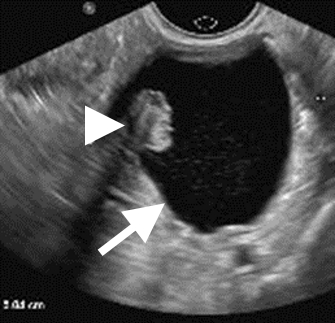
Figure 3.a. Incidentally noted 5cm non-simple cyst (arrow) on CT containing a mural solid component (arrowhead) in a post-menopausal woman. Such a lesion should be imaged further with transvaginal US or MRI. b. US image shows a unilocular cyst (arrow) with a mural nodule (arrowhead).
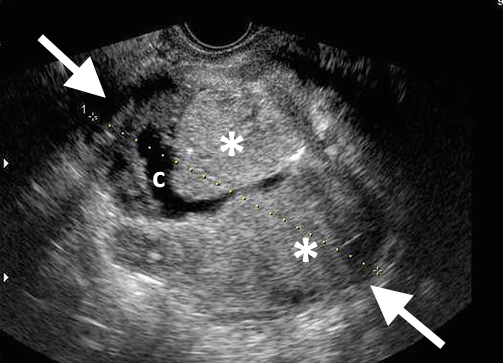
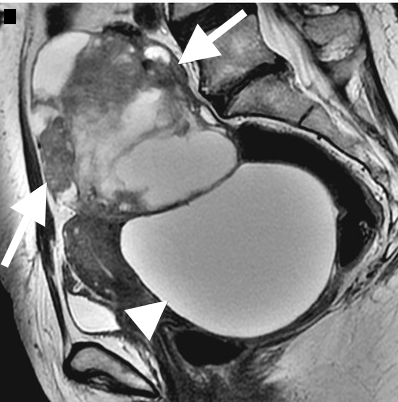
Figure 4.a. US showing an ovarian mass that is mostly solid (*) with cystic component (c) in a pre-menopausal woman; solid components were vascular on Colour Doppler US (not shown here). b. Sagittal T2-weighted MR image in a different post-menopausal patient showing a large complex ovarian mass (arrows) above the bladder (arrowhead). Both lesions a and b were confirmed to be ovarian cancers.
References
- Ghosh E, Levine D. Recommendations for adnexal cysts: have the Society of Radiologists in Ultrasound consensus conference guidelines affected utilization of ultrasound?. Ultrasound quarterly 2013;29(1):21–24. 2.
- Hermans AJ, Kluivers KB, Janssen LM, et al. Adnexal masses in children, adolescents and women of reproductive age in the Netherlands: A nationwide population-based cohort study. Gynecologic oncology 2016;143(1):93–97.
- Levine D, Patel MD, Suh-Burgmann EJ, et al. Simple Adnexal Cysts: SRU Consensus Conference Update on Follow-up and Reporting. Radiology 2019;293(2):359–371.
- Andreotti RF, Timmerman D, Strachowski LM, et al. O-RADS US risk stratification and management system: A consensus guideline from the ACR ovarian-Adnexal Reporting and Data System committee. RADIOLOGY 2020;294(1):168-185.
- Patel MD, Ascher SM, Horrow MM, et al. Management of Incidental Adnexal Findings on CT and MRI: A White Paper of the ACR Incidental Findings Committee. JACR 2020;17(2):248–254.
- Wang PS, Schoeck OG, Horrow MM. Benign-appearing Incidental Adnexal Cysts at US, CT, and MRI: Putting the ACR, O-RADS, and SRU Guidelines All Together. Radiographics 2022;42(2):609–624.
- Patel MD. Invited Commentary: Categorizing Adnexal Masses at US, CT, and MRI-the Radiologist’s Not-Impossible Mission. Radiographics 2022;42(2):E77–E79.

