Migraine
Dr Naomi Piscopo & Dr Maria Cauchi
ABSTRACT Migraine is a very common neurological disorder affecting people from numerous age groups and it has been a subject for ongoing research over the past years. Studies have described vascular and neurological pathways as well as cortical spreading depression as being the underlying mechanisms responsible for the symptomatology of the disorder. Multiple triggers have been implicated, out of which genetic susceptibility is very significant. The varied clinical picture of migraine has led to the development of various forms of management ranging from non-specific to very specific preventive, acute and chronic treatment.
Keywords: Vascular and Neurological Mechanisms, Cortical Spreading Depression, Genes, Migraine Management
Introduction
Migraine is classified as a primary headache disorder which manifests as recurrent painful headache attacks. These attacks differ in frequency amongst individuals and also in duration ranging from an hour up to even three days. The prevalence is higher in females (18%) than in males (6%).1 Generally, the onset of migraine is seen at around puberty, with the onset of menarche in females, with its effects peaking between the ages of 35 and 45 and declining thereafter.2
Pathophysiology
The pathophysiology of migraines is best described through an interaction of vascular and neurogenic theories hence making the disorder of neurovascular origin. Thomas Willis described how the pain experienced from the headache is a result of vasodilation of the meningeal and cerebral arteries.3 It was later established that there is an interaction between the brain’s neural activity and the mentioned blood vessels. Migraine is known to be associated with hypertension, stroke, and a patent foramen ovale, hence confirming the role of the vascular system in its pathophysiology.4
In 2013, Amin et al conducted imaging studies during spontaneous migraine attacks and concluded that the dilation of blood vessels is not the principal cause of central and peripheral pain.5 It is the proinflammatory agents as well as neuropeptides released from trigeminal nerve afferents within the meninges that trigger the pain. This occurs together with the vasodilation via sensitization of both the central and peripheral neurons in the trigeminovascular system.6 Genetic variability is an important component that influences the susceptibility of developing this problem, as well as the severity of the symptoms.7
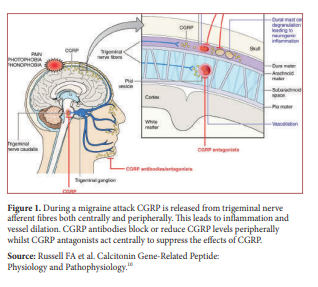
The trigeminal nerve and its fibres innervate a set of intra- an extra- meningeal blood vessels and this is what makes up the trigmeninovascular system.8 Nerve endings from this system innervate both intracranial and extracranial structures such as venous sinuses and the eye respectively. During the pain phase of the condition the trigeminovascular system is activated and initiates a cascade of events from the sensory nerve endings of the trigeminal nerve. Vasoactive neuropeptides such as substance P, calcitonin gene-related peptide (CGRP), pituitary adenylate cyclaseactivating peptide, neurokinin A and nitric oxide are usually stored in the trigeminal nerves.9 When released, they lead to vasodilation and increased blood flow which result in oedema in the meningeal vascular system further worsening the sensation of pain as demonstrated in Figure 1.10 Furthermore, upon stimulation of the trigeminal nerve system, structural changes of the dura mater have been noted including mast cell degranulation as well as changes in the postcapillary venules such as platelet aggregation.11
Another important phenomenon is linked to migraine aura; the cortical spreading depression (CSD) was first described in 1943 by a Brazilian neurophysiologist.12 This is an electrophysiological event described as an intense wave of neurological activity within the brain at a rate of 2-5mm/min which slowly spreads over cortical brain regions and precedes a prolonged period of depressed neural activity as it interferes with calcium, potassium and sodium ion gradients.13 It has been proven that CSD activates the trigeminovascular system hence contributing to the pain.14 CSD is implicated in visual aura where the visual field is affected, starting at the centre and spreading to the periphery at a rate of 3mm/min.15
Aetiology
Migraine has a strong genetic component, also stemming from the interaction which multiple genes – particularly those concerned with neural, vascular, hormonal and mitochondrial systems – have with environmental factors.7 Genes coding for serotonin and dopamine systems have been studied and an association has been identified between the human serotonin transporter SLC6A4 gene and migraine. The latter gene codes for a membrane protein that removes serotonin from the synapse and recycles it back into neurons.16 During a migraine attack, serotonin levels are known to be decreased and this leads to neuropeptide release. Dopamine’s interaction with its receptors in the trigeminovascular system is implicated in the prodromal symptoms experienced.17 A range of food items have been identified as triggering factors and include chocolate, alcohol, cheese and dairy products.18 The fact that migraine attacks are more common in women post-puberty may be explained by the fluctuating levels of female hormones during the menstrual cycle which interact with oestrogen and progesterone receptors, rendering females more susceptible. Both during pregnancy and post-menopause, hormonal levels are relatively constant and it is during these times that migraine episodes decrease.19 Other known triggering factors include exercise, the oral contraceptive pill and variations in the sleep-wake cycle.
Symptoms and Signs
The typical presentation of migraines is of a severe unilateral headache which may be pulsatile. Nausea, vomiting and photophobia are commonly associated features.20 There may also be allodynia, lacrimation, ptosis, depression and transient amnesia.21 Before a patient experiences the headache, there may be a prodrome and an aura which arise from areas in the cortex, brainstem, hypothalamus and limbic system. The prodromal phase consists of symptoms which precede the headache by several hours and include food cravings, irritability, and fatigue.20 The migraine aura is a separate phase of a migraine attack consisting of focal neurological symptoms which last from five minutes till one hour before migraine headache onset and then resolves completely. Symptoms and signs may be positive or negative indicating gain-offunction or loss-of-function respectively. Examples include tremor or muscle weakness if the motor cortex is affected or flashing lights and scotomas when the somatosensory cortex is involved. Aphasia will result if the speech area is affected.22
Management
The non-pharmacological management of migraine includes reassessment of the patient’s diet and lifestyle. Therapy sessions including relaxation and cognitive behavioural therapy have also been proven useful.23 NSAIDs and other simple analgesics, such as paracetamol, together with the anti-emetic metoclopramide may also be used during an acute migraine episode.24 The more specific anti-migraine drugs include ergot and triptan derivatives which demonstrate agonistic properties on serotonin receptors and are also used in the acute phase. Locally, Zolmitriptan is the triptan mostly in use. The release of neurotransmitters from central and peripheral trigeminal nociceptive nerve terminals can be inhibited by the serotonin-5HT1B/1D receptor agonist zolmitriptan as well as ergot alkaloids, and indomethacin.25 Triptans exert their effect by causing intracranial vasoconstriction and also reduce neuropeptide extravasation.23 Studies have proved the benefit of using combinations of NSAIDs and triptans to improve outcome.26 Although the majority of patients do not require preventive medication, this should be considered if the patient’s quality of life is significantly affected, if there are frequent attacks and in case of unresponsiveness to acute treatment. Amongst the most effective and preventive drugs in use is the beta-blocker propranolol which has been showed to reduce migraine frequency by more than 50%. Tricyclic antidepressants particularly amitriptyline, calcium channel blockers including verapamil and flunarizine as well as antiepileptic medications such as carbamazepine, gabapentin, valproic acid and topiramate are also used.27 Modern treatment under development entails the use of humanized monoclonal antibodies against CGRP and its receptors which are implicated in the pathophysiology of migraine.28 More complex targeted therapy for migraine is brain modification; transcranial magnetic stimulation is one example where brain excitability is modified.29
Conclusion Migraine episodes have consequences on the patient’s quality of life as it may interfere with employment, their capability to take care of their families and social relationships. This may be measured using the Migraine Disability Assessment where higher scores are associated with greater levels of disability.30 Given the complexity of the condition, research and studies are on the increase so as to gather more knowledge and hence be able to understand and manage this debilitating disease better.

