Imaging Cancer of the Rectum: The importance of accurate staging in treatment planning
Dr Pierre Vassallo
Colorectal cancer is the third most common cancer in men and the second most common in women worldwide.1 It is the third leading cause of death in both sexes. The prevalence is higher, while mortality rate is lower in developed countries. However, there has been an increasing prevalence in patients under 50 years of age, and in these cases the mortality rate is also increasing.2,3
The prognosis of rectal cancer is directly related to tumour involvement of the mesorectum and the ability to achieve complete resection with tumour-free margins.4 The ability of MRI to depict the the mesorectum and the extent of its involvment by the tumour has significantly improved treatment planning and outcomes. Figure 1 shows the rectum surrounded by the mesorectum, the latter being delimited by the mesorectal fascia (MRF). The most effective treatment for rectal cancer is complete surgical excision of the mesorectum, also known as Total Mesorectal Excision (TME). For tumours involving the MRF, also known as Locally Advanced Rectal Cancers, neoadjuvant chemoradiotherapy can be used to shrink the tumour prior to TME. It is important to note that the mesorectum thins out as it extends inferiorly and is absent at the level of the anal sphincters.
Neoadjuvant chemoradiotherapy results in a significant tumour downstaging in around half the patient treated, while in almost a third of patients complete resolution of the tumour is observed. In the latter cases, some authors recommend follow-up with no surgical intervention.
Thus MRI of the rectum is used to distinguish patients who can go directly to surgery from those who would benefit from neoadjuvant chemoradiotherapy. In addition, it allows assessment of the effectiveness of neoadjuvant chemotherapy, tailored surgical planning and post-operative follow-up/restaging for tumour recurrence.5 Poor prognostic factors such as extramural vascular invasion and mucin content can also be detected by MRI.
Figure 2 describes the staging rectal cancer based on MR findings, where T refers to tumour size/extent, N relates to the extent of lymph node disease and M refers to the presence and extent of distant metastases.6 T1, T2 and T3a and b tumours are treated directly with TME. T3c and d combined with N1 lesions receive short term radiotherapy followed by TME. T3 MRF+, T4 or N2-staged lesions receive neoadjuvant chemotherapy and long term radiotherapy followed by a restaging MRI scan.
There are different types of TME, which are based on the distance of the tumour from the anal sphincters. For tumours located in the upper and middle rectum, a low anterior resection is performed, which preserves the inferior portion of the rectum and anal sphincters and allows colorectal anastomosis. An ultra-low anterior resection may be possible in inferior rectal tumours, in which the colorectal anastomosis is performed 1cm below the tumour margin. For tumours less than 1cm from the anal verge an abdominal perineal (AP) resection is employed with excision of the anus and sphincters and formation of a permanent colostomy. An intersphincteric AP resection may be possible with sparing of the external sphincter. For more extensive tumours that infiltrate the external sphincter or levator ani muscles, an extraelevator AP resection may be performed which includes a broader dissection of the perineal muscles.
MRI staging of rectal cancer is based on Fast Spin Echo T2-weighted images without fat suppression. These provide clear distinction between the bowel wall layers, mesorectal fat and mesorectal fascia. The axial planes assess extent of invasion of bowel wall layers (Fig 3). Sagittal and coronal images depict the level of the tumour (upper, mid or lower rectum: 10.1-15cm, 5.1-10cm and 0-5cm from the anal verge) (Fig 4a). Coronal images are also used to assess involvement of the internal or external anal sphinters (Fig 4b). Infiltration of the anterior peritoneal reflection, which is the peritoneum extending between the rectum and uterus or bladder, raises the tumour stage to T4a (Fig 5a). While infiltration of adjacent organs such as the prostate (Fig 5b) or seminal vesicles increases tumour stage to T4b.
Additional imaging sequences may be used in restaging including Diffusion- Weighted Imaging (DWI) with B-value >800secs/mm2 (Fig 6a) or contrast-enhanced fat-satuated T1-weighted imaging (Fig 6b). These imaging sequences are not required in the initial staging of rectal cancer, but they are useful for assessing residual tumour after chemoradiotherapy or surgery and for detection of tumour recurrence.
The above article provides but a superficial overview of the capabilities of MRI in staging rectal cancer. Numerous important details relating to imaging finding and staging of rectal cancer have been omitted here for the purpose of maintaining simplicity. More extensive and specific literature on the capabilities of MRI for rectal cancer staging is included in the references section. MRI of the rectum is an established and indispensible tool for staging rectal cancer and for monitoring response to therapy.
Figure Legends
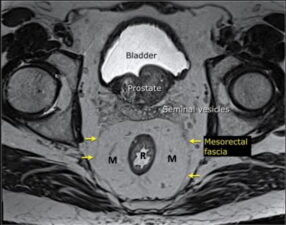
Figure 1. The mesorectum (M) surrounds the rectum (R) and is delimited by the Mesorectal Rectal Fascia (arrows).

Figure 2. TNM staging of rectal cancer. T refers to Tumour size/extent, N relates to the extent of lymph Node disease, M refers to the presence and extent of distant Metastases.
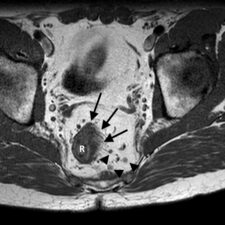
Figure 3. Para-axial T2-weighted MR scan through the rectum (R) showing >5mm infiltration into the mesorectum (arrows) and >3 suspicious mesorectal lymph nodes (arrowheads) (Stage T3cN2). Case courtesy of Dr Natalie Yang, Radiopaedia.org, rID: 6990.
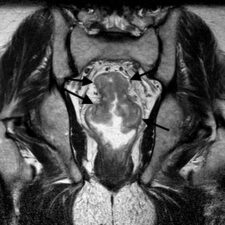
Figure 4a. Coronal image T2-weighted MR scan through the rectum showing a rectal cancer (arrows). The level of the cancer is best assessed on sagittal and coronal images. Case courtesy of Dr Natalie Yang, Radiopaedia.org, rID: 7124.

Figure 4b. Sparing of the internal (I) and external (E) anal sphincter is best confirmed on coronal T2-weighted images. (T – tumour) Case courtesy of Dr Natalie Yang, Radiopaedia.org, rID: 7124.
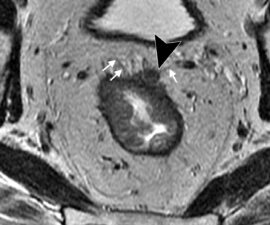
Figure 5. Infiltration of the MRF, peritoneum and adjacent organs can be assessed with axial T2-weighted images. a. Infiltration of the peritoneal reflection (arrowhead) between the bladder and rectum (arrows) (stage T4a).
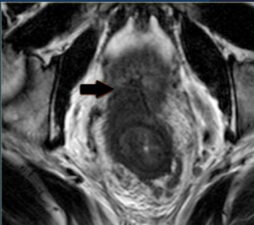
b. Infiltration of the prostate (arrow) (stage T4b).
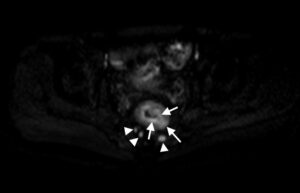
Figure 6a. Transverse DWI image with high B-value taken through the mid-rectum following chemoradiotherapy shows areas of residual tumour as bright areas within the rectum and mesorectum (arrows) as well as in involved lymph nodes in the mesorectum (arrowheads) (Stage T3N1). Case courtesy of Dr Natalie Yang, Radiopaedia.org, rID: 7135.
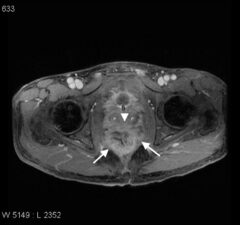
Figure 6b. Contrast-enhanced fat-saturated T1-weighted scan of the rectum following chemoradiotherapy showing tumour invading beyond the mesorectum (arrows) and the prostate (arrowhead) (P – prostate) (Stage T4b) Case courtesy of Dr Natalie Yang, Radiopaedia.org, rID: 6989.
References
- Ferlay J, Soerjomataram I, Dikshit R et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer2015; 136(5): e359–e386.
- American Cancer Society. Cancer facts and figures: 2018. – https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2018/cancer-facts-and-figures-2018.pdf. Accessed 19 Nov 2019.
- Bailey CE, Hu CY, You YN et al. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg2015;150(1):17–22.
- Nagtegaal I, Gaspar C, Marijnen C, et al. Morphological changes in tumour type after radiotherapy are accompanied by changes in gene expression profile but not in clinical behaviour. J Pathol2004;204(2):183–192.
- Horvat N, Tavares Rocha CC, Oliveira BC et al. MRI of Rectal Cancer: Tumour Staging, Imaging Techniques, and Management. RadioGraphics2019; 39(2):367-387
- https://cancerstaging.org/references-tools/quickreferences/Documents/ColonSmall.pdf

