Endometrial Imaging
Pierre Vassallo
The endometrium demonstrates a wide spectrum of normal and pathologic appearances throughout menarche as well as during the prepubertal and postmenopausal years and the first trimester of pregnancy. Characteristic morphologic changes take place in the uterus and endometrium over time.
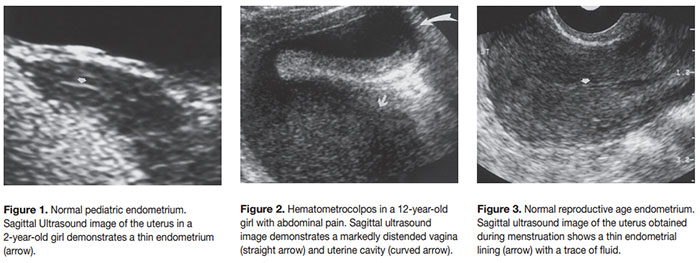
At birth, the uterine body is smaller than the cervix, and the endometrium generally appears as a thin, echogenic line (Fig 1). However, fluid may be present in the uterine cavity; this is due to the effects of transplacental maternal hormones.
The most common endometrial abnormalities in neonates include hydrocolpos and hydrometrocolpos. Hydrocolpos is characterized by distention of the vagina and hydrometrocolpos is characterized by dilatation of both the uterine cavity and vagina with serous fluid and sometimes urine if a vesico-vaginal fistula is present. Both hydrocolpos and hydrometrocolpos in neonates result from cervical or vaginal stenosis, hypoplasia or agenesis.
In contrast, hematocolpos and hematometrocolpos in adolescent girls are generally associated with an imperforate hymen without an increase in associated congenital anomalies. Ultrasound demonstrates an echogenic, tubular, cystic midline mass with internal echoes representing fluid and debris (Fig 2).
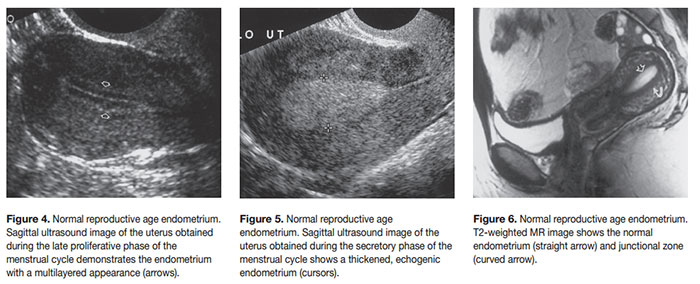
During the reproductive age, the appearance of the endometrium will change with the phase of the menstrual cycle. This is best analysed on endovaginal scans. During menstruation, the endometrium appears as a thin, echogenic line 1–4 mm in thickness. Endometrial thickness is measured from echogenic border to echogenic border across the endometrial cavity on a sagittal midline image (Fig 3). During the proliferative phase of the menstrual cycle (days 6–14), the endometrium becomes thicker (5–7 mm) and more echogenic relative to the myometrium, reflecting the development of glands, blood vessels, and stroma. In the late proliferative (periovulatory) phase, the endometrium develops a multilayered appearance with an echogenic basal layer and hypoechoic inner functional layer, separated by a thin echogenic median layer arising from the central interface or luminal content (Fig 4). In this stage, the endometrium may measure up to 11 mm in thickness. The layered appearance usually disappears 48 hours after ovulation. During the secretory phase, the endometrium becomes even thicker (7–16 mm) and more echogenic (Fig 5). This increased echogenicity is thought to be related to stromal edema and glands distended with mucus and glycogen. The endometrium typically reaches a maximum thickness during the midsecretory phase. The appearances of normal and abnormal endometrium, such as in the setting of endometrial hyperplasia, may overlap, so imaging of the endometrium is best performed during or immediately following menstruation.
The MR imaging appearance of normal endometrium during the reproductive age is best demonstrated on T2-weighted images. T2-weighted images delineate the uterine zonal anatomy. The normal endometrium is of uniformly high signal intensity, with the inner myometrium, or junctional zone, of uniformly low signal intensity and the outer myometrial layer showing higher signal intensity than the inner layer (Fig 6).
Transvaginal Ultrasound is the primary modality for evaluation of an early intrauterine pregnancy, which varies in appearance depending on gestational age. At 4.5 weeks gestation, the normal gestational sac appears as an oval or rounded anechoic space measuring 5mm in diameter located within the endometrium and surrounded by a hyperechoic rim at least 2 mm in thickness. The sac should grow at a rate exceeding 1.2 mm per day (Fig 7). The yolk sac should be visualized between 5 and 6 weeks gestation, and an embryo may be seen before 6 weeks gestation. The gestational sac should be located in the upper or middle uterine segment, midway between the two apposed uterine walls. A low position in the endometrial cavity suggests an impending or ongoing miscarriage, a cervical ectopic pregnancy, or a fundal fibroid compressing the sac downward. The presence of placental blood flow on Color Doppler Ultrasound in a cervical ectopic pregnancy or low-lying sac is useful in distinguishing these entities from an abortion in progress.
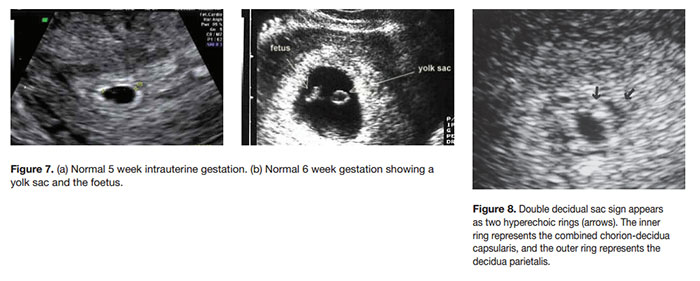
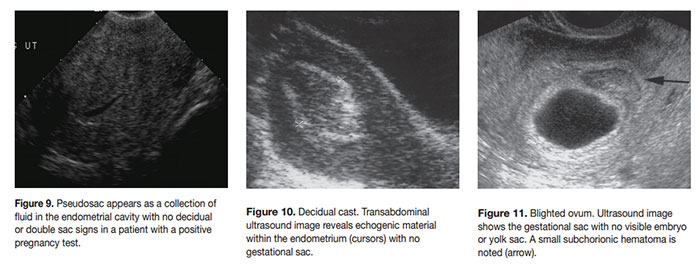
The hyperechoic ring surrounding the gestational sac represents the decidual reaction before 5 weeks of gestation. After 5 weeks gestation, a double decidual sac sign may be seen, the inner sac representing the choriondecidua capsularis and the outer layer the decidua parietalis (Fig 8). Both the decidual and double decidual signs help distinguish a normal intrauterine pregnancy from a pseudosac that may occur in up to 20% of ectopic pregnancies (Fig 9). Prior to visualization of a yolk sac or embryo, these two Ultrasound signs assist in the diagnosis of a normal intrauterine pregnancy.
Apparent endometrial thickening in the setting of a positive pregnancy test may in fact represent an echogenic decidual cast in the endometrium (Fig 10), although retained products of conception may have a similar appearance. A decidual cast is suggestive of an ectopic gestation. A thin decidual reaction of less than 2 mm, an abnormally shaped sac, or a gestational sac in a low uterine location suggests an abnormal pregnancy. An empty gestational sac may represent a blighted ovum, particularly when the mean gestational sac diameter is >10 mm (Fig 11). A blighted ovum is an anembryonic gestation.
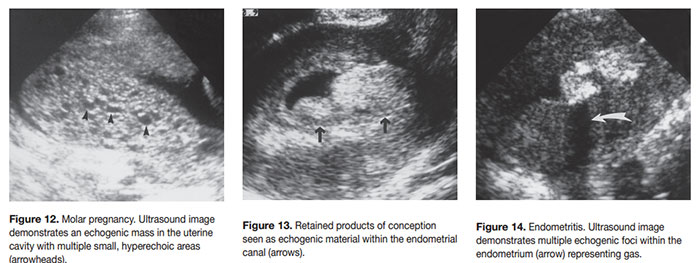
Gestational trophoblastic disease is a proliferative disease of the trophoblast that may manifest as a complete or partial hydatidiform mole, invasive mole, or choriocarcinoma. A hydatidiform mole, the most common form of gestational trophoblastic disease, is noninvasive and usually manifests in the second and third trimesters. This type of mole distends and fills the endometrial cavity without invading the myometrium. Ultrasound demonstrates a uterus that is enlarged for gestational age and filled with multiple small, hyperechoic areas 3–10 mm in diameter with posterior acoustic enhancement (Fig 12). The cysts represent grossly swollen villi from trophoblastic hyperplasia.
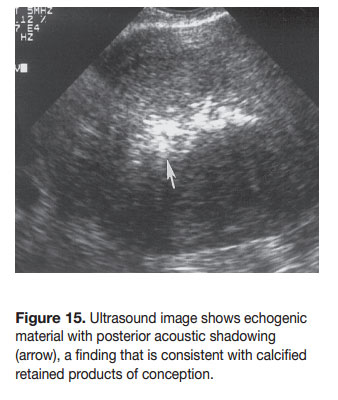
Normal ultrasound findings in the postpartum uterus include uterine enlargement and an endometrial cavity less than 2cm in thickness. The cavity wall has a variable appearance ranging from smooth, well-defined borders to irregular, heterogeneous linings, with considerable overlap between normal and abnormal cases. Small echogenic foci within the endometrial cavity may not be pathologic. Abundant intrauterine echogenic material may however represent retained products of conception (Fig 13), while the presence of gas bubbles may indicate endometritis (Fig 14), the latter being more common after caesarian section. Air in the uterus may be present in up to 20% of normal postpartum women, so clinical findings must also be considered when considering treatment. Retained products of conception that are seen late after delivery may contain calcifications (Fig 15).