Detecting Breast Cancer – Advanced and New Technologies
Pierre Vassallo
This has consequently generated considerable interest in the literature with the result that Breast Cancer Screening Programs have become available in most developed countries. The aim of these screening programs is to achieve early detection of breast cancer in women who have not yet developed any symptoms. Such early detection allows early treatment, which is necessary to achieve a good treatment outcome. Treatment of early cancer results in cure in 98% of cases, while late cancer detection results in a poor outcome.
Early breast cancer detection depends on the accuracy of the equipment used and on training and experience of the specialists involved. Equipment accuracy and consequently image quality play a very important role since specialist training and experience cannot compensate for poor image quality. New technologies are contributing to improved image quality and also to new parameters that help distinguish benign from malignant disease.
Mammography is the mainstay of breast cancer screening particularly for women who are 40 years of age or older; these women have a significantly higher risk of developing breast cancer. Ultrasound (US) is used for screening younger women particularly those who are 35 years of age or less. Both mammography and breast US are frequently combined in women over 40 years of age with an improvement in diagnostic confidence and accuracy. Further evaluation with breast Magnetic Resonance Imaging (MRI) and image-guided biopsy is required when abnormal findings are present.
There have been dramatic improvements in mammographic technology in recent years. Film-screen mammography, which used chemically-processed film to record images of the breast, has been largely replaced by digital mammography since the latter methods deliver better image quality and require less exposure to radiation. Digital mammography uses two different technologies, computed radiography (CR) or full field digital mammography (FFDM).
CR mammography uses a fluorescent plate that is subsequently scanned to obtain an image of the breast. FFDM acquires an image of the breast through an array of tiny solid state detectors, which are more efficient than the fluorescent plate resulting in much better image quality (Figure 1) and a further reduction in radiation exposure.
Breast US is used as a first line for breast imaging in younger women due to the absence of ionizing radiation and the limitations mammography has in dense breasts. Image quality in breast US has greatly improved over time. Characteristics detected on standard (B mode) US have been shown to be highly accurate for distinguishing cancerous from non-cancerous disease (Figure 2). Color Doppler imaging has been shown to help further in characterizing breast lesions and for guiding biopsy.
US elastography is a new technology that is being introduced to improve detection and characterization of breast masses. There are two types of US-elastography available. Strain elastography is used to evaluate how a lesion deforms when it is compressed. Lesions that are soft deform more than those that are stiff and the strain elastography scale provides a qualitative measure of the amount of tissue stiffness (Figure 3). Shear-wave (SW) elastography uses an US push pulse to generate shear waves. SW velocity (Vs) in the tissue is proportional to the square root of stiffness (Young modulus) of the lesion. This allows quantitative evaluation of tissue stiffness. Hard lesions are mostly benign, while softer lesions, which show more deformability on strain elastography and higher Vs values on SW elastography, are more likely to be malignant. Strain elastography has been shown to significantly improve accuracy for distinguishing cancer from non-cancerous lesions. SW elastography is less accurate than strain elastography due to artefacts, but a number of design improvements are currently being tested, which will likely change the situation.
MRI has been widely used for detecting and assessing breast lesions. MRI is sensitive for detecting breast cancers, with a sensitivity as high as 100% for invasive breast cancers, and therefore has emerged as an adjunctive breast imaging modality to mammography and US. MRI has limitations in lesion characterization, but it is still useful in conjunction with mammography and US for differentiating between benign breast lesions and benign-looking breast cancers. It is of particular value for evaluating dense breasts. Important indications for breast MRI include a positive BRCA 1 or BRCA 2 test or a 1st degree relative BRCA+, patients who have had prior radiotherapy to the chest wall, individuals with > 25% lifetime risk based on genetic models (some of which take breast density into consideration), for problem solving (e.g. post-operative breasts with distortion) and to search for synchronous, multifocal or multicentric disease. High T2 signal, flow restriction on Diffusion Weighted Imaging (DWI) and/or strong and rapid contrast uptake with sustained enhancement or early washout are features of malignant disease (Figure 4).
Breast imaging has developed into a complex algorithm composed of a variety of modalities all of which contribute to accurate detection and staging of cancer. Continued specialist training and constant upgrading to new and improved imaging technologies are necessary to provide the best image quality needed to guide optimal breast cancer management.
| All technologies mentioned above are available at DaVinci Health |
Figure Legends
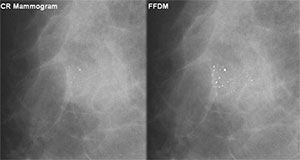
Figure 1. The presence of microcalcifications may be one of the earliest signs of breast cancer on mammography. Left (CR) and right (FFDM) mammograms show the same cluster of microcalcifications, but depiction on FFDM is far superior.
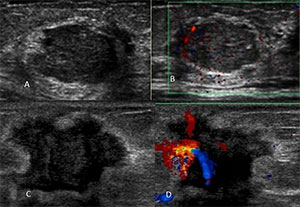
Figure 2. Image A shows an ultrasound image of a benign nodule (fibroadenoma) showing smooth margins while Image B is a color Doppler image of the same lesion showing a lack of blood vessels. Image C is an ultrasound image of an invasive ductal cancer demonstrating irregular margins with abundant blood flow shown on the color Doppler image (D).
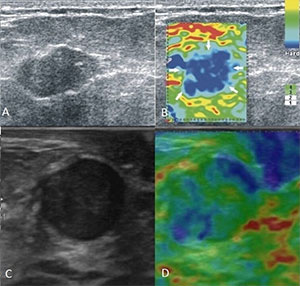
Figure 3. Image A shows a lesion with slightly irregular margins and showing abundant internal echoes that on conventional US might be suggested it to be benign. However Image B shows this to be a very “blue” lesion, which indicates a hard nodule and is strongly suggestive of malignant disease. This lesion was confirmed through biopsy to be an invasive ductal cancer. Image C depicts a rounded lesion with low echogenicity and smooth margins, however it lacks blue colour on elastography (Image D) suggesting a rather soft lesion; this was confirmed on biopsy to be a fibroadenoma, which is benign.
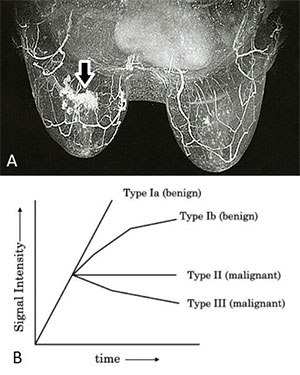
Figure 4. Image A shows a contrast enhanced T1-weighted fat suppressed image of both breasts with an enhancing mass (arrow) in the right breast that was histologically confirmed to be an invasive ductal cancer. Image B shows the enhancement patterns that are characteristic of benign and malignant lesions.

