Certification and Monitoring of Deaths During the COVID-19 Pandemic
DR KATHLEEN ENGLAND, PROF. NEVILLE CALLEJA
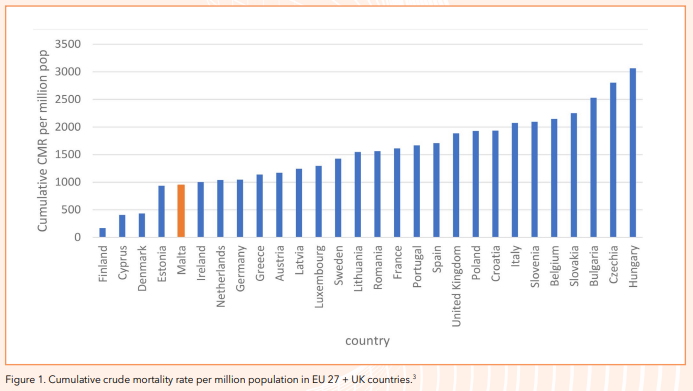
INTRODUCTION The SARS CoV-2 pandemic which began late in 2019 has caused and continues to cause much morbidity and mortality worldwide. It was declared a pandemic by WHO on 11 March 2020.1 Up to 26 May 2021 there has been 167,848,565 reported cases of COVID-19 worldwide and 3,485,787 reported deaths.2 Malta reported its first case locally on 7 March 2020 and its first death a month later, on 8 April 2020. Though geographical disparities in incidence of COVID-19 are evident across the globe, the geographical distribution of COVID-19 deaths shows even wider disparities between some continents and also between countries.3,4 However the situation is still evolving all the time, with unprecedented cases and deaths being currently observed in India. At an EU level (+ the United Kingdom) cumulative crude mortality rate due to COVID-19 per million population in Malta compares well with the other member states as per figure 1.
Different measures and indicators are being used to monitor the COVID-19 situation in different countries. These aim to guide policy and decision-making based on trends within the country as well as comparison with other countries. International Organisations such as WHO and the European Centre for Disease Control have issued guidelines and standard definitions aimed at standardising as much as possible data reported by different countries world-wide.
This paper aims to review the common mortality indicators in place with a special emphasis on the situation in the Maltese Islands.
OVERALL MORTALITY
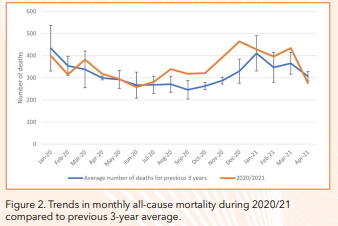
If one looks at monthly trends from all deaths locally from January 2020 till April 2021 compared to the previous 3-year average (figure 2), significant increased mortality is mainly observed from August 2020 reaching a peak in November and December 2020. Mortality figures returned to expected levels of previous years in April 2021. COVID-19 mortality as seen further down in the article follows this pattern with the peak in COVID-19 deaths also observed in a similar period.
However monthly mortality data only gives an overall indication of trends in mortality and often information and data which is needed during the pandemic needs to be available in a more timely – often daily – frequency.
COVID-19 DEATHS
The collection of mortality data on COVID-19 deaths is one of the important epidemiological indicators used to assess the disease situation in a country as well as to monitor public health interventions and gauge how well the health care system is coping.1
Early in June 2020, WHO issued guidelines on how the medical cause of death section should be completed for COVID-19 related deaths. According to the WHO guidelines, COVID-19 should be reported on all death certificates where the ‘disease caused or contributed to the death’. However, this should be reported specifying the causal sequence of events and with as much detail as possible. The use of official terminology i.e. COVID-19 should be used for all certification of this cause of death. The use of ‘coronavirus’ in place of COVID-19 is not recommended as there are many types of coronavirus.5 The aim of these guidelines is to assist countries to report COVID-19 deaths correctly, allowing standardisation of mortality data collection as much as possible.
Despite WHO guidelines, different countries count COVID-19 deaths differently. This also depends on resources available to count COVID deaths and reliability of certification which depends not only on the compilation of the death certificate but also on testing and diagnostic resources available.
According to a briefing by the European Parliament published in July 2020, although all EU member states report COVID-19 deaths, the definition of what constitutes a ‘COVID-19 death’ may vary from country to country.6 Further to this, at a death certification level, differences in reporting may relate to the time frame that a COVID-19 death may be accepted as such, distinguishing between deaths which are primarily or secondary due to COVID-19, distinguishing between confirmed and suspected COVID-19 deaths and other sources of heterogeneity which makes effective comparison even at an EU level difficult.6 Reporting of COVID-19 deaths also depends on cases being diagnosed in the first place which may depend on the testing capacity within the country.
In keeping with the above, in another study which compared 6 EU countries,7 apart from differences in testing capacity between the countries and also differences in the stages of the pandemic the countries were in, differences were also observed in reporting of deaths and death certification which may lead to differences in the observed number of deaths due to COVID-19 reported. In some countries it is at the discretion of the certifying doctor as to whether to order a COVID-19 test posthumous especially for deaths in care homes and in the community, and there is a cost involved which is not covered by insurance. Differences were also observed in how and where COVID-19 was put down on the death certificate, as well as the transfer of this information to the authorities involved, with some countries using electronic death certification while other countries using a number of different sources of information to determine the number of COVID-19 related deaths. Under-reporting of deaths due to COVID-19 especially in care homes and in the community has also been highlighted in some countries especially earlier on in the pandemic.7
Since COVID-19 often causes death among the elderly with several co-morbid conditions it may be challenging to decide on the causal chain of events leading to the death of a patient as there may be a number of competing causes of death.
When comparing COVID-19 deaths between countries, it is very important to compare like with like. Apart from the issues highlighted, choosing the best mortality indicator to allow comparability is also very important but this depends also on data availability. Whilst the number of deaths may be a useful measure for one country, this has very limited scope for comparing different countries. Other measures which are used include the crude mortality rate which describes the number of deaths per population; however, this does not take into account the age structure of the population. Great variations in age structure between countries will not allow valuable comparisons and were possible, standardised rates should be used. Other issues which also must be taken into consideration include the ‘stage’ of the pandemic the country is in and also the often imbalance found between different regions of the same country affected by COVID-19.8
Locally from the start of the pandemic high testing rates were deemed to be of utmost importance as a measure to control the disease.9 Testing took place in hospitals, residential homes and community and was free of charge. Persons who died suddenly, and cases were there was any suspicion of COVID-19, underwent a PCR test after death. All confirmed deaths where COVID-19 was either a primary or secondary cause of death were coded in a timely manner; when queries arose as to whether COVID-19 was considered a primary or secondary cause of death, these were discussed with the certifying physician. Locally a confirmed death due to COVID-19 is one in which the patient had a positive laboratory test for and died due to COVID-19 or its complications. COVID-19 related deaths are reported on a daily basis.
From the beginning of the pandemic to date (26/05/2021), Malta reported 419 COVID-19 related deaths. COVID-19 was considered as the underlying cause of death in 85% of cases while in the remaining 15% COVID-19 was considered as a contributory cause. Malta reported few COVID deaths in the first wave of the pandemic and from week 15 up to week 22 there were only 9 reported COVID-19 deaths. This was followed by a lull, however increasing deaths were then observed from week 34 (figure 3) with a peak in deaths observed in November and December 2020.
EXCESS DEATHS FROM ALL CAUSES
Another important mortality indicator often used to monitor deaths during the pandemic is what is known as ‘excess deaths’. In simple terms one compares the mortality experienced during a specific time period in the country or region against the average of example the last 5 years or some other baseline. The advantage of this indicator is that it does not depend on testing availability in the country or cause of death certification which may be either under or over-reported, as all deaths are included. Excess deaths also serve to monitor trends and is often available more rapidly in some countries than deaths by cause. Another advantage of monitoring excess mortality is that since mortality in a specific country is compared with itself in previous years, it is not affected by differences in age structure and other factors in different countries.10
A study carried out in Portugal during the first few months of the pandemic found that there were 14% excess deaths of which 49% were directly related to COVID-19 and 51% were due to other causes. The study supports the idea that some COVID-19 deaths may not have been reported or were missed, however it also reports that patients who were suffering from other acute medical conditions may have been afraid to access hospital care due to the pandemic. The study also states that the reduction of traffic deaths during this period due to COVID-19 restrictions could have led to some compensation of excess deaths from the other causes.11
Because of these advantages, excess mortality monitoring is sometimes viewed as ‘the gold standard’ when comparing deaths. However, as with other indicators it too has its drawbacks. Measuring excess mortality is not possible in all countries. In order to be effective, real time or close to real time data must be available, as well as comparative data for previous years. Also, excess mortality does not give information on the cause of the excess’ e.g. during the COVID-19 pandemic health care facilities may have not been able to cope and treat effectively patients needing hospitalization due to other causes because of the excessive influx of patients with COVID-19, resulting in possibly excess deaths from other causes. On the other hand, measures implemented during the COVID-19 pandemic may have resulted in a decrease in deaths which are usually observed e.g. decrease in influenza deaths which compensated for the increased deaths from COVID-19, so the true excess deaths due to COVID-19 is masked.8
Malta has been monitoring excess deaths on a weekly basis through its membership with the European Mortality Monitoring system called EuroMOMO12 since 2009. EuroMOMO has the overall objective to monitor in real time excess deaths due to influenza and other public health threats across 27 European countries who are currently members of this network. Other countries are also encouraged to join the network. The advantage of being a member of EUROMOMO is that comparable, standardised monitoring of excess mortality is available on a weekly basis. Trends in mortality across these 27 European countries by number of deaths, age group and z-scores are available for all countries in an aggregated manner, while at individual country level z-scores allow comparative analyses to be done between countries and are updated on a weekly basis and available on the EuroMOMO website. The z-score relates to the standard deviation from the norm (mortality expected) during that period of the year. A standard deviation > 2 represents excess mortality, with values > 2 and ≤ 4 representing low excess in mortality and scores > 4 and ≤ 7 representing moderate excess in mortality, etc.
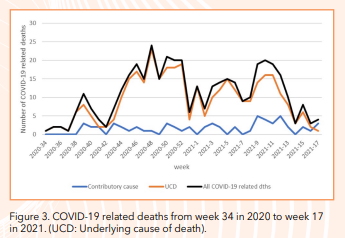
Figure 4 shows the weekly number of excess deaths for all ages and all causes of death from week 34 in 2020 to week 18 in 2021 in Malta, compared to similar periods in the previous two years. Excess mortality exceeding 20 deaths or more per week is considered significant. Significant excess deaths were consistently observed from week 44 to week 52 in 2020, quite comparable to the peaks in COVID-19 deaths observed in figure 3. In the first weeks of 2021 a peak in excess mortality is observed similar to that in the previous two years. In previous years (2018-19, 2019-20) this was due to the influenza season as well as cold weather. January 2021 observed few, if any, influenza deaths locally, but we were still observing a number of COVID-19 deaths. The 75-84 year age group accounted for 38% of all excess mortality, followed by the 85+ age group which accounted for 32% of all excess deaths and the 65-74 year age group which accounted for 23% of all excess deaths.
As seen in figure 4 quite a sharp decrease in excess mortality is observed from week 12 onwards and can be attributed to the high COVID-19 vaccine uptake among the elderly and vulnerable populations who were prioritised and started being vaccinated first, late in December 2020.
CASE FATALITY RATIO
Another indicator which is often quoted is the case fatality ratio (CFR), sometimes referred to as the case fatality rate. WHO defines this as the ‘proportion of deaths (due to COVID-19) among identified confirmed cases (of COVID-19)’.13 CFR is an important indicator as it reflects the severity of the disease under investigation.14
Another indicator which is sometimes used is the infection fatality ratio. This represents the true measure of the severity of the disease and is the total number of deaths from COVID-19 divided by the number of infected individuals. However, this often can only be estimated using serological testing on a representative random sample of the population, due to the substantial proportion of persons in which infection can be subclinical or asymptomatic; this may be costly and time consuming.13
However, there are a number of limitations when using the CFR. Apart from issues related to the variations in counting of COVID-19 deaths as outlined previously, another issue which will affect it is that severe cases of COVID-19 who are still alive but will die later will be counted as cases but not as deaths leading to underestimation of the CFR.3 The denominator can also vary substantially between countries according to what criteria are used to test individuals for COVID-19. In countries which mainly allow testing for hospitalised or very symptomatic patients will overestimate the CFR as those who are tested are often more severely sick and could possibly die compared to the mildly symptomatic or asymptomatic cases who are less likely to be tested and therefore not included in the denominator.15 Also, especially in the beginning of the pandemic or when countries were overwhelmed, the limited testing capacity of some countries may have resulted in missed cases and deaths.14 Further to this, in some countries, underprivileged sectors of society may have limited access to healthcare and testing, and testing outside hospital facilities may be against payment.
CFR varies between countries and regions and it also varies according to the stage of the pandemic; it can also be calculated by different age groups and according to pre-existing medical conditions.3 However, because of the limitations and variations outlined above one needs to be very careful how this measure is used especially when comparing different countries. The highest CFR documented in Malta was on 28 December 2020 (1.73%). This was also the time where the mortality rate from COVID-19 was highest locally. Currently it has stabilized at 1.37% (24/05/2021) compared to the EU average which is currently 2.25%.3

Two other measures proposed to overcome the limitations of CFR are 1) individuals’ survival probability which depends on the availability of individual data and, 2) number of deaths due to COVID-19 as a proportion of number of deaths + number of recovered persons from COVID-19; however some bias still remains on the utilisation of these two measures. 13,15
POLICY IMPLICATIONS
While the importance of gathering timely data and information has been highlighted during this pandemic, the correct interpretation of data presented is essential in order for it to serve health policy.10 Also it is very important that an indicator is interpreted in light of the bigger picture in terms of both all other indicators available to monitor the pandemic, and also in respect to the local and international situation, public health measures and strain on the healthcare system. Consideration of the impact of the pandemic on the wider aspects of society is also needed to make the best decisions possible for the good of the population.
The death certification process as well as the monitoring of deaths during the pandemic needs to be viewed as part of a larger health monitoring system as well as part of the public health response available. This pandemic also serves to highlight the challenges relating to accessing real-time data, as well as the need for the implementation of measures to collect data which is of better quality. Malta has one National Mortality Register which captures all deaths occurring on the Maltese Islands and also has good communication channels with certifiers and public health policy makers which allowed the timely verification of all COVID-19 related deaths. However, there is always room for improvement and currently an important project that is being developed locally by the Public Registry Unit of Identity Malta is the ‘electronic death certificate’ which will allow the instant transfer of death certificates and allow even more timely monitoring of deaths.
Data on various COVID-19 indicators are available from a number of international sources10 which are updated very frequently; however, understanding the limitations of the different data sources should always be considered when interpreting and understanding the data. The Institute for Health Metrics and Evaluation16 has very recently updated its method of calculating total mortality due to COVID-19 based on excess deaths but taking into account ‘drivers of change in mortality…. since the onset of the pandemic’.
These drivers which need to be taken into account include possible increases in other causes of death due to, example, delay in accessing health care, as well as decrease in other causes of death e.g. influenza. As highlighted by the Institute there is great heterogeneity between countries in deaths due to COVID-19 and also gross underestimation in some countries between what is reported and the estimated mortality due to COVID-1916 More work is needed locally to dissect excess mortality experienced during the pandemic into the different causes of death, however trends in COVID-19 related deaths and excess mortality followed a similar pattern to date.
Monitoring of the impact of the COVID-19 pandemic goes beyond the time we are living in now when the virus is still rampant and causing havoc across the world. Its impact on the health, social and economic sphere is still developing and needs close surveillance to be able to implement needed policies in hard hit areas.
ACKNOWLEDGMENTS:
Ms Connie Scicluna and Ms Desiree D’Amato who work on the National Mortality Register.
REFERENCES
- National Center for Health Statistics. Guidance for certifying deaths due to COVID–19. Hyattsville, MD. 2020.
- Johns Hopkins: Corona Virus Resource Center [Internet]. Johns Hopkins University & Medicine. [cited 26 May 2021]. Available from: https:// coronavirus.jhu.edu/map.html
- Ritchie H, Ortiz-Ospina E, Roser M, et al. Coronavirus Pandemic (COVID-19) [Internet]. Our World in Data. 2020 [cited 26 May 2021]. Available from: https://ourworldindata.org/coronavirus
- Poorolajal J. Geographical Distribution of COVID-19 Cases and Deaths Worldwide. J Res Health Sci 2020;20(3):e00483.
- World Health Organization. International guidelines for certification and classification (coding) of COVID-19 as cause of death based on ICD International Statistical Classification of Diseases. April 2020. Avaialbel from: https://www.who.int/classifications/icd/Guidelines_Cause_of_ Death_COVID-19.pdf?ua=1
- European Commission. Assessment of COVID-19 surveillance case definitions and data reporting in the European Union. July 2020. Available from: https://www.europarl.europa.eu/RegData/etudes/ BRIE/2020/652725/IPOL_BRI(2020)652725_EN.pdf
- West A, Czypionka T, Steffen M, et al. Reporting of COVID-19 deaths in Austria, France, Germany, Italy, Portugal and the UK, Social Policy Working Paper 10-20, London: LSE Department of Social Policy. 2020. Available from: https://www.lse.ac.uk/social-policy/Assets/Documents/PDF/ working-paper-series/10-20-Anne-West.pdf
- Villani L, McKee M, Cascini F, et al. Comparison of Deaths Rates for COVID-19 across Europe During the First Wave of the COVID-19 Pandemic. Front Public Health 2020;8:620416.
- Micallef S, Piscopo TV, Casha R, et al. The first wave of COVID-19 in Malta; a national cross-sectional study. PLoS One 2020;15(10):e0239389.
- Corrao G, Rea F, Blangiardo GC. Lessons from COVID-19 mortality data across countries. J Hypertens 2021;39(5):856-860.
- Vieira A, Peixoto VR, Aguiar P, et al. Rapid Estimation of Excess Mortality during the COVID-19 Pandemic in Portugal -Beyond Reported Deaths. J Epidemiol Glob Health 2020;10(3):209-213.
- Institute SS. EUROMOMO [Internet]. [cited 25 Apr 2021]. Available from: https://www.euromomo.eu/
- World Health Organization. Estimating mortality from COVID-19: scientific brief, 4 August 2020. Available from: https://apps.who.int/iris/ handle/10665/333642.
- Lin TPH, Wan KH, Huang SS, et al. Lam DSC. Death tolls of COVID-19: Where come the fallacies and ways to make them more accurate. Glob Public Health 2020;15(10):1582-1587.
- Böttcher L, Xia M, Chou T. Why estimating population-based case fatality rates during epidemics may be misleading. Preprint. medRxiv 2020;2020.03.26.20044693. Published 2020 Mar 30.
- Institute for Health Metrics and Evaluation. Estimation of total mortality due to COVID-19 [Internet]. 6 May 2021. [cited 9 May 2021]. Available from: http://www.healthdata.org/special-analysis/estimation-excessmortality-due-covid-19-and-scalars-reported-covid-19-deaths

