BI-RADS Guide to the Non-Specialist – Understanding the Breast Specialist’s Jargon
Dr Pierre Vassallo
According to the American Cancer Society, approximately one in eight women will develop breast cancer during their lifetime. This is why breast cancer screening has become so important and why it is being given so much attention by healthcare planners. A standardised and evidence-based protocol for breast cancer screening and breast cancer management is needed to optimise treatment outcomes. This has been the driving force behind the development of BI-RADS, which stands for Breast Imaging Reporting and Data System.
In the past, the medical jargon used for describing imaging findings on mammograms, was highly non-standardised and was influenced by personal preference. This often led to miscommunication and sometimes even mismanagement due to misinterpretation of communicated results.
These factors led to efforts that started in the late 1980s aimed at standardising mammographic terminology and reporting. In 1993, the first edition of the BI-RADS lexicon was issued by the American College of Radiology.
The advantages of using BI-RADS are as follows:
- It allows standardised, rational and structured analysis of the breast
- Reporting nomenclature is standardised, which avoids confusion
- It facilitates communication between breast specialists and clinical staff involved in the management of breast cancer patients to enhance management
- It facilitates monitoring of treatment outcomes
- It facilitates education of breast care specialists.1
The BI-RADS mammography lexicon is presently in its 5th edition and it is regularly revised based on experience and learning.2 Meanwhile, BI-RADS lexicons have also been developed from Breast Ultrasound and for Breast MRI, both now in their 2nd edition.
While BI-RADS is mainly used by breast care specialists, a basic understanding of its significance is also important for patients and their care-givers. It allows them to understand their breast imaging results and helps them participate in their treatment.
A standard mammography report should follow a standard structure:
- It should start with a statement indicating why the mammogram is being performed (screening or to follow-up a previously detected lesion) and the date/s of the previous exam/s to which the present one is being compared.
- The next statement should indicate the breast type, which is classified based on the balance between fatty and fibro-glandular components into four types: predominantly fatty, patchy fibroglandular elements, heterogeneously dense breast and very dense breast (Figure 1). Breasts are considered very dense if they contain a lot of fibro-glandular tissue (>75%) and little fat (Type 4), while they are classified as fatty if they contain mostly (> 75%) fat (Type 1). Breast density is important for several reasons. Dense breast tissue may increase a woman’s chance of developing breast cancer.3 Also, detection of breast cancer using mammography is more difficult in women with dense breasts. The American Cancer Society estimates that approximately 80% of women fall in one of the middle two categories, while 10% have fatty breasts and another 10% have very dense breasts.
- If an abnormality is noted on a mammogram:
- Its location should be recorded based on laterality, quadrant and clockface location, depth and distance from the nipple (Figure 2), and
- Its characteristics should be described,
- Any change in size or characteristics from previous exams must be reported.
- A BI-RADS classification is then issued based on descriptors listed in 3.
- Finally, Management recommendations are made.
Section 3 in the mammogram report can only occur if an abnormality since it involves description of the lesion’s characteristics; this forms the basis of the BI-RADS classification. BI-RADS scores are as follows:
BI-RADS 0: Need for further imaging or comparison with previous exams
BI-RADS 1: No abnormalities
BI-RADS 2: Benign findings
BI-RADS 3: Probably benign but cannot totally exclude malignant disease
BI-RADS 4: Suspicious findings (groups A, B and C based on increasing level of suspicion)
BI-RADS 5: Findings strongly suggestive of malignant disease
BI-RADS 6: Biopsy-proven breast cancer undergoing treatment
Lesion description is a complex exercise as the features being analysed often lie along a continuous spectrum of change rather than in clearly distinct subgroups. Here are the main lesion feature groups defined in the BI-RADS lexicon:
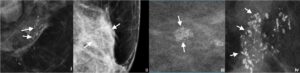
- Asymmetries: these are densities seen only in one projection or lack clear convex border on one projection. They may be focal (in less than one quadrant) (Figure 3a) or global (occupying one quadrant or more)(Figure 3b). Focal asymmetries are often due to tissue superimposition, while global asymmetries are usually normal variants. Of more concern is the developing asymmetry, which shows growth or change in shape over time; 15% of these are cancers (Figure 3c).
- Mass lesions: these are 3-dimensional lesions that are clearly seen on 2 projections and that have convex borders. They are described based on size, shape (Figure 4) and margins (Figure 5), density of nodule (low/intermediate/high) and associated findings.
- Associated findings: these include calcifications (Figure 6), associated distortion (Figure 7), duct changes (Figure 8), skin thickening and/or retraction (Figure 9).
There are many situations where there is no clear BI-RADS score that matches the imaging findings. Here are some of these situations:
- In very dense breasts with no imaging findings but poor visibility, one must score as BI-RADS 1. However, one must also recommend or proceed to further imaging such as ultrasound and in some cases MRI.
- All stable intramammary lymph nodes, benign calcifications, fat-containing lesions, implants or metallic artefacts, known benign architectural distortion (clear stability over time) are classified as BI-RADS 2.
- A score of BI-RADS 3 should be used only if findings are almost certainly benign (<2% suspicion). A radiologist should not use BI-RADS 3 if he/she is not sure. If a radiologist is unsure about a finding (>2% suspicion), a BI-RADS 4A score should be used and further investigation recommended; this may involve a follow-up mammogram or breast ultrasound within 6 months. Increase in size of the lesion should prompt biopsy, while decrease in size or development of benign features should reclassify the lesion to BI-RADS 2. Stable lesions should be followed with imaging.
- Unilateral axillary lymphadenopathy that is clearly benign based on mammographic findings should be classified as BI-RADS 2. If not clearly benign, this finding should be given a BI-RADS 0 score and further investigation with ultrasound should be performed. One must consider the possibilities of an occult breast cancer, lymphoma or metastatic carcinoma (such as from melanoma, other skin cancer or ovarian cancer).
- Bilateral axillary lymphadenopathy with no breast findings should be classified as BI-RADS 2 even if the patient has known lymphoma, since the BI-RADS classification is based only on findings present in the breast. However, an additional statement must be included in the recommended management section of the report stating the presence of lymphadenopathy and its underlying cause.
- If a patient has had breast cancer resection with positive resection margins (i.e. incomplete resection), but mammograms show only post-op change, a BI-RADS 2 score should be used. However, a statement relating to surgical resection margins must be included in the management statement.
- In a case of clinically evident Paget’s disease of the nipple (cancer of the nipple) with no suspicious mammographic findings, one must issue a BI-RADS 2 score and add a statement about the nipple findings in the recommendations section.
- BI-RADS 0 scores should be avoided particularly if a benign-appearing lesion is present or if further imaging with breast MRI is required.
The significance of the BI-RADS classification lies in the relationship between the BI-RADS score and likelihood of malignant disease. The following statistical associations have been demonstrated:
BI-RADS 1 – 0% malignancy
BI-RADS 2 – 0% malignancy
BI-RADS 3 – 0-2% likelihood of malignancy
BI-RADS 4 – A 2-10% risk; B 11-50% risk; C 51-95% risk
BI-RADS 5 – >95% risk
BI-RADS 6 – Biopsy-proven malignancy under treatment
The BI-RADS classification is one of the main diagnostic tools that guides management. Significant discrepancies between pathology and BI-RADS reports do sometimes occur, and it is often the BI-RADS report that dictates further management and not the pathology report as the latter may be influenced by sampling errors.
In conclusion, the BI-RADS score and management recommendations help the breast radiologist to guide treatment and follow-up and ensures accurate communication between all breast care specialists. In addition, the BI-RADS classification provides a system for structured/systematic reporting that is particularly beneficial for training new breast radiologists. Finally, a basic understanding of the classification helps patients understand and participate in their own treatment.
Figure Legends

Figure 1. Breast Type as seen on mammography: a. predominantly fatty breast, b. a breast containing scattered fibroglandular elements, c. a heterogeneously dense breast, and d. a very dense breast.
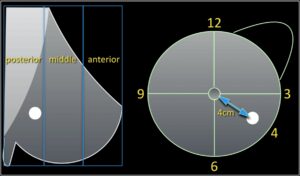
Figure 2. Lesion location reporting must include side, quadrant (upper outer, upper inner, lower outer, lower inner), clockface location (e.g. 0700), depth (anterior, middle, posterior) and distance from nipple in centimetres.
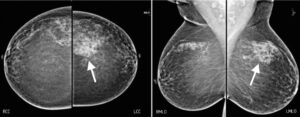
Figure 3. a. Focal asymmetry (arrow) appears as a denser area in less than one quadrant with no clear convex borders; this asymmetry was confirmed to be normal glandular tissue on ultrasound.
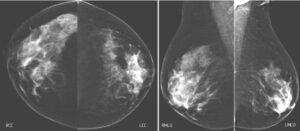
b. Global asymmetry with the right breast containing more fibroglandular tissue than the left over an area larger than one quadrant; this is frequently a normal variant.

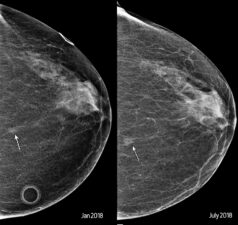
c. Small asymmetry (arrow) noted in an 80 year old woman that shows growth and change in shape when reviewed 6 months later.

Figure 4: Lesion shape is classified into 3 groups: round (a), oval (b) or irregular (c). Round and oval lesions are mostly benign, while irregular lesions raise a high degree of suspicion.

Figure 5: Lesion margins are classified into 5 types: circumscribed (a), obscured (b), micro-lobulated (c), indistinct (d) and spiculated (e). Type a represents the lowest level of suspicion, while type e represents the highest suspicion for malignant disease.
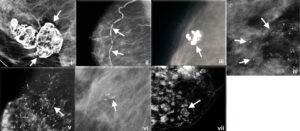
Figure 6: Calcifications within a lesion are classified based on their shape and size. a. Benign type calcifications may have the following features: macro (>1mm), central lucency (i), vascular (ii), popcorn (iii), rounded and numerous (<1mm) (iv), solid rods (v), milk of calcium (vi) and egg-shell (vii) shape. All aforementioned forms of calcification are classified as BI-RADS 2 or 3.
b. Malignant-appearing calcification are given a BI-RADS 4 classification. These include fine linear/branching/fragmented (i), pleomorphic (mixture of appearances) (ii), amorphous (iii) and coarse heterogeneous (iv).
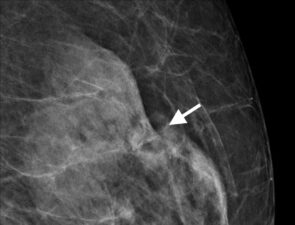
Figure 7: Architectural Distortion refers to any distortion of the tissue texture lines within the breast (arrow).
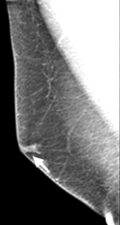
Figure 8: A solitary dilated duct (arrow) is sometimes seen on a mammogram particularly in the case of a fatty breast. In the absence of associated suspicious calcifications, this represents <2% risk for malignancy.
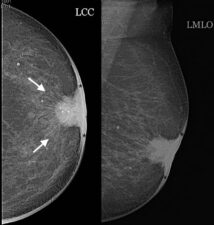
Figure 9: Spiculated retroareolar lesion (arrows) with associated skin thickening (*) due to infiltration of the nipple and adjacent skin.
References
- Pesce K, Orruma M, Hadad C, et al. BI-RADS Terminology for Mammography Reports:
What Residents Need to Know. Radiographics 2019: 319-320.
- D’Orsi C, Sickles E, Mendelson E, et al. Breast Imaging Reporting and Data System: ACR BI
RADS breast imaging atlas (5th ed.). Reston, Va: American College of Radiology; 2013.
- McCormack V A, dos Santos Silva I. Breast Density and Parenchymal Patterns as Markers of
Breast Cancer Risk: A Meta-analysis. Cancer Epidemiol Biomarkers Prev 2006; 15(6): 1159
1169.

