Treating Gastro-oesophageal reflux disease (GERD) with sense
Edgar Pullicino MD DCH FRCP ( Lond & Glasg) PhD
Consultant Gastroenterologist
Treat now, test later
A therapeutic trial of a high dose twice daily proton pump inhibitor (PPI) (taken before food to increase acid suppression and with good compliance) will lead to partial or complete relief of suspected acid reflux – related symptoms (e.g. heartburn, cough), in the majority of unselected cases. Gastro oesophagoscopy is mandatory in patients with alarm symptoms (e.g. dysphagia, weight loss) and is advisable in patients with chronic reflux symptoms to exclude Barrett’s oesophagus (fig 1), a columnar epithelial metaplasia with an increased risk of progression to dysplasia and oesophageal carcinoma that necessitates regular endoscopic surveillance. PPIs rarely reverse this condition but may decrease its cancer potential and they allow the pathologist to assess dysplasia better by abolishing inflammatory atypia.
When PPIs “fail”
Endoscopic appearances of low-grade (fig. 2) or high-grade (fig. 3) oesophagitis are highly diagnostic of GERD and predict symptomatic relief by PPIs but symptoms often recur on withdrawing PPIs. Ironically, a less satisfactory group to treat are those patients with a normal endoscopy (non erosive reflux disease: NERD, see fig 4). About 60% of NERD patients will obtain complete symptom relief on single dose daily PPIs. Only 5% of non-responders will show significantly abnormal 24 hour oesophageal pH monitoring patterns during twice daily PPI treatment. Indeed, multichannel intraluminal impedance probes correlate episodes of non-acid reflux with symptoms in these patients. Biopsies from NERD patients exhibit marked widening of the spaces between the squamous epithelial cells lining the lower oesophagus that allow pepsin, refluxed duodenal bile acids and other noxious agents to sensitize oesophageal submucosal nerve endings. NERD patients have a higher pain sensitivity to short duration reflux episodes that those with erosive oesophagitis.
A sub group of these NERD patients have normal pH studies off PPI and are classified as having functional heartburn. Many of these patients show pain hypersensitivity to physiologic amounts of acid exposure and to minor oesophageal distension. Not surprisingly they obtain limited relief from high dose PPIs. Another NERD subgroup do not show any correlation between acid reflux episodes during ambulatory pH monitoring and pain. They have a visceral hyperalgaesia to low intensity stimuli which are totally unrelated to reflux events and will not respond to PPI. Alginates, prokinetic agents and life style changes may be tried but central pain modulators such as tricyclic antidepressants are more likely to bring relief.
PPIs on demand?
Given that endoscopically proven NERD rarely progresses to an erosive oesophagitis, it makes economic and practical sense to step down from empiric double-dose PPI therapy to single dose PPI therapy or to intermittent (doctor-driven) or on-demand (patient-driven) PPI regimens. Studies have shown that compliance to once daily PPI regimen is poor in well patients who often pursue an on-demand approach.
When necessary, long-term PPI therapy is safe. PPIs reduce the usual acid-induced inhibition of gastrin secretion by the antral “G” cells. The resultant mild hypergastrinaemia may cause hyperplasia of the enterochromafin-like (ECL) cells but progression from hypertrophy to dysplasia or to gastric carcinoid neoplasia, which has been observed in rats on high doses of PPIs, does not occur in humans. Acid suppression does allow mild bacterial overgrowth to occur in the upper intestine but again no untoward effects have been observed.
Helicobacter pyloric (Hp) and GERD: strange bed fellows
Gastric Hp colonization causes focal atrophic gastritis in the body of the stomach, destroys parietal cells and reduces acid output. Eradication of this natural biologic antisecretory agent could, in theory, worsen GERD or Barrett’s oesophagus and induce oesophageal adenocarcinoma. Many gastroenterologists would choose to eradicate gastric Hp in an attempt to prevent the progression of atrophic gastritis to metaplasia and carcinoma although large-scale population-controlled studies of potential cancer prevention are not available. Hp-related duodenal or gastric ulcer (past or present) or Hp-related low grade primary B-cell MALT lymphoma require HP eradication.
Non medical treatment
Patients who persist with severe heartburn, regurgitation or aspiration despite PPIs or who refuse long term PPIs, may be considered for antireflux surgery after extensive investigation using endoscopy, oesophageal monitoring, gastric emptying studies and 24 hour pH testing. Functional heartburn, gastroparesis, achalasia and scleroderma must be excluded. The presence and size of a hiatus hernia should be assessed radiologically. The most popular operation is a laparoscopic (Nissen) fixation and wrapping of the gastric fundus around the lower oesophagus. Dysphagia and gas-bloat may result from to tight a plication. The operation is not always superior to PPIs in the long term and rarely cures Barrett’s oesophagus
Endoscopic therapeutic options include endoscopic suturing, silicon injection and radiofrequency (RF) treatment. RF treatment is achieved using a cooled (Stretta®) balloon (fig 5) with retractable barbs that are deployed after endoscopy to apply current at various level to the LES. This treatment is reported to good give long-term relief but is not recommended for use in patients with a large hiatus hernia or Barrett’s oesophagus.
Management of the GERD patient should be guided by an understanding of the interaction between abnormalities of anatomy or motility, patterns of acid/pepsin exposure and the corresponding responses in the oesophageal mucosa. Rational management can be planned after appropriate investigations using endoscopy, biopsies and more specialized techniques where necessary.
Legends to Figures

Fig 1: Barretts oeophagus
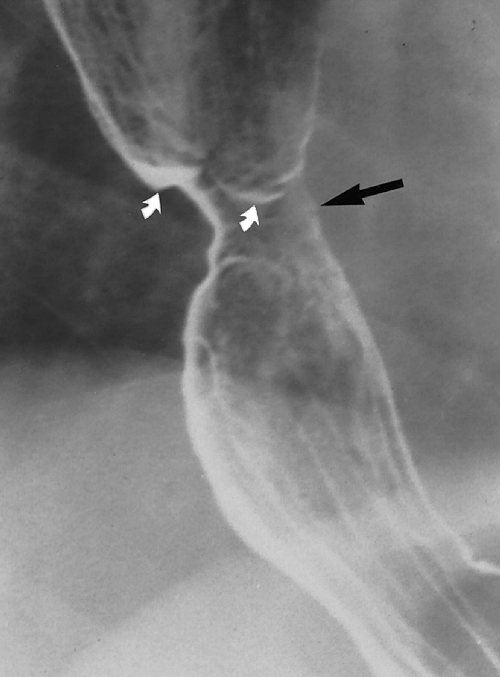
Fig 2: Mild oesophagitis

Fig 3: Severe oesophagitis
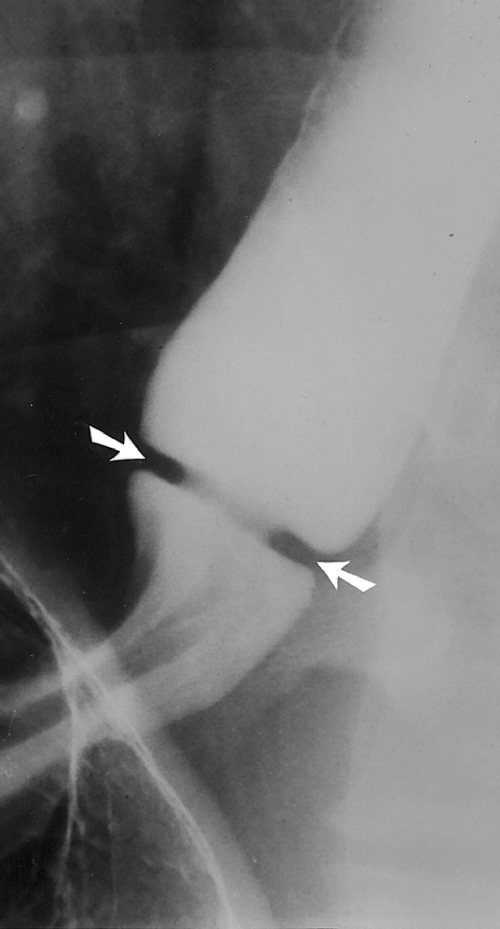
Fig4: Normal lower oesophagus
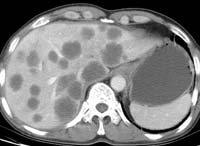
Fig 5: Stretta ® device

