Rotator Cuff Surgery Saves Society Money
Surgery to repair torn rotator cuffs improves patients’ quality of life and can allow them to get back to work quickly, resulting in societal savings for patients 61 years and younger, according to a new analysis led by Duke Medicine.
 “Two thirds of patients who undergo surgery for torn rotator cuffs are of working age. Productivity for working people is critically important, and our study demonstrated that in patients with rotator cuff tears, getting people back to work quickly and effectively pays for the cost of the surgery itself,” said lead author Richard C. Mather III, M.D., assistant professor of orthopaedics at Duke Medicine.
“Two thirds of patients who undergo surgery for torn rotator cuffs are of working age. Productivity for working people is critically important, and our study demonstrated that in patients with rotator cuff tears, getting people back to work quickly and effectively pays for the cost of the surgery itself,” said lead author Richard C. Mather III, M.D., assistant professor of orthopaedics at Duke Medicine.
The findings were published in the Journal of Bone & Joint Surgery.
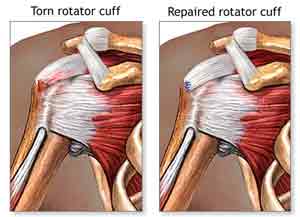
According to recent studies, approximately 4.5 million people visit the doctor each year with shoulder pain. A range of injuries and disorders affect the rotator cuff, a group of muscles and tendons attached to the shoulder joint that stabilize the shoulder and allow it to move.
When the rotator cuff is torn, both surgery and nonoperative treatments, such as physical therapy, medication and steroid injections, can improve the injury’s symptoms and outcomes.
Few studies have examined the financial burden of rotator cuff tears and the economic impact of treatment is largely unknown. Societal costs of a medical condition include direct costs associated with the diagnosis and treatment, as well as indirect costs. Indirect costs can include probability of employment, household income, missed workdays and disability payments.
“Indirect costs are important factors, but they are often left out of health economic evaluations due to the difficulty in measuring these costs,” Mather said. “However, these costs are critically important in musculoskeletal care where the goal is very often to improve function and quality of life to allow patients to return to a productive lifestyle.”
Using mathematical modeling, the researchers evaluated lifetime direct and indirect costs associated with surgery and other treatments for rotator cuff tears. They analyzed data for patients ages 30 to 80 with full-thickness rotator cuff tears who either underwent surgery or opted for nonoperative treatment. Mather said the researchers measured quality-of-life in 95 patients from Rush University Medical Center, and estimated indirect costs using data from 73 patients from the Rothman Institute/Jefferson Medical College.
Estimates for direct costs for both surgery and nonoperative treatments were based on the national average reimbursement for public and private payers. Indirect costs were calculated using a model developed by a team of health economists led by Lane Koenig, Ph.D., of KNG Health Consulting. The model utilizes survey data and patient-reported outcomes to estimate indirect costs for a condition.
The researchers found that the societal savings from rotator cuff surgery compared with nonoperative treatment was $13,771 over a patient’s lifetime. When multiplied by the approximately 250,000 rotator cuff repairs performed in the United States each year, the estimated lifetime societal savings was $3.44 billion. Surgical treatment also resulted in a significant improvement of quality-of-life measurements.
“While surgery is not necessary for all patients, we found a wider range of outcomes among people who had nonoperative treatment,” Mather said. “A systematic review of the literature supported our assumption that 68 percent of patients will respond to nonoperative treatment. However, model simulations found that the indirect costs of not having access to surgery for those 32 percent that do not respond are extremely high, and drive the overall mean cost savings of rotator cuff repair.”
Cost savings were highly sensitive to age, with savings ranging from $77,662 for people 30 to 39 years old to $11,997 for those 70 to 79 years old. The reduced indirect costs resulting from surgery more than offset the costs of surgery in patients 61 years old and younger. For people over 61 years of age, societal costs for surgery exceeded those for nonoperative treatment, but surgery still remained a cost-effective option based on improvements in quality of life.
Although rotator cuff surgery was found to save money for younger patients, the findings do not suggest that all rotator cuff tears require surgery, as nonoperative treatment is often preferred. The researchers hope that the study will help doctors begin to distinguish between patients who would benefit more from surgery versus nonoperative treatment.
“The ultimate solution is not to say that everyone should or should not have surgery, but to take these findings and personalize them to maximize the value for each individual patient,” Mather said.
This study is part of a larger effort to determine the value of musculoskeletal interventions and protect access to treatments for high-risk patients who would benefit most from interventions that may have substantial upfront direct costs. The overall aim is to provide complete information for decision-makers to ensure that healthcare resources are allocated efficiently.
Source Newsroom: Duke Medicine

