MR Imaging of early Rheumatoid Arthritis and Spondyloarthropathy – Part II
Pierre Vassallo
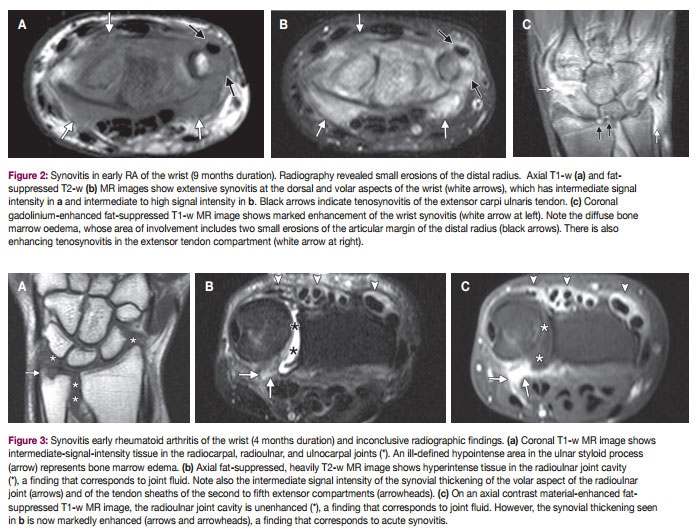
Bone marrow oedema may be seen alone or surrounding bone erosions (Fig 2-3) and is considered to be a potentially reversible phenomenon. Histologic studies of joint replacement specimens have shown that bone marrow oedema corresponds to inflammatory cellular infiltrates in the bone marrow, representing osteitis. Bone marrow oedema is considered to be a very early marker of inflammation, given that its presence correlates with increased levels of acute phase reactants (erythrocyte sedimentation rate and C-reactive protein) and the clinical stage of disease activity. Bone marrow oedema is also closely related to the degree of synovitis and has been associated with subsequent erosive damage; as a result, it is currently considered to be a ‘forerunner’ of erosions
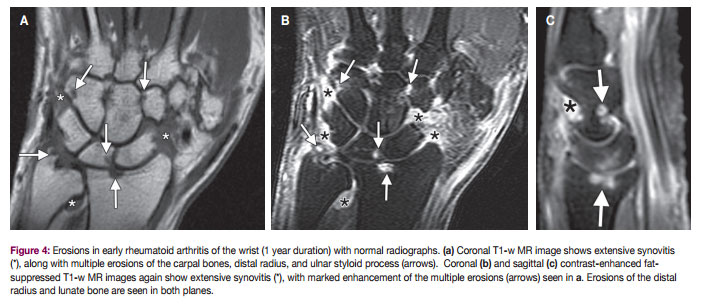
The detection of erosions in patients with early rheumatoid arthritis is a key imaging finding, since it indicates irreversible joint damage. On radiographs, the presence of erosions is suggested by the loss of visualization of the bone cortex. MR imaging helps detect more bone erosions in the wrist and hand in early rheumatoid arthritis (Fig 4) than does radiography. In early rheumatoid arthritis, MR imaging helps identify bone erosions in 45–72% of patients with disease of less than 6 months duration, compared with 8–40% for radiography. It is also important to identify those patients with early rheumatoid arthritis in whom progressive disease is not seen, since aggressive treatment may not be required in such cases. Indeed, 82% of patients without erosions at baseline MR imaging had no radiographic erosions at 2-year follow-up.
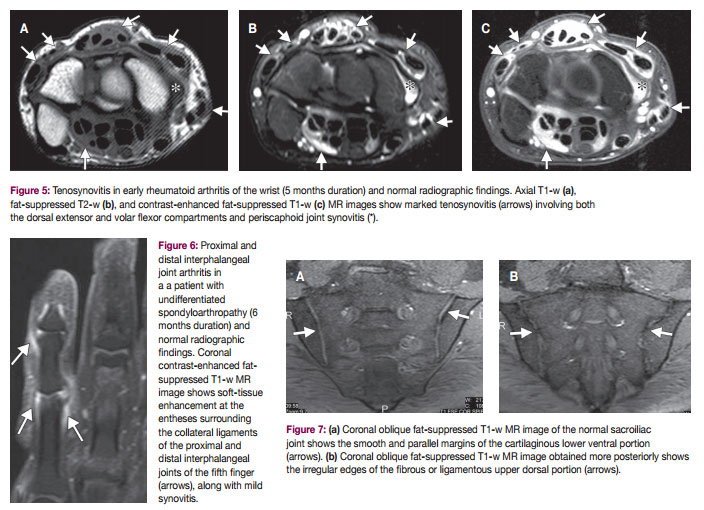
Tenosynovitis is commonly seen in early rheumatoid arthritis of the wrists and hands. MR imaging signs of tenosynovitis include fluid in the tendon sheath, increased thickness or contrast enhancement of the tendon sheath synovium, or a combination thereof (Fig 5). If tendon sheath fluid is minimal, this may be a normal finding, however contrast enhancement of the same sheath is confirmatory of tenosynovitis.
Spondyloarthropathies involving peripheral joints, particularly psoriatic polyarthritis, may pose problems in the differential diagnosis from RA. This is especially true in cases of psoriatic arthritis without psoriatic skin lesions. Radiographic changes in psoriatic arthritis appear late compared to those on MR imaging. Unlike rheumatoid arthritis, there is usually extensive involvement of the DIP joint in psoriatic arthritis. The distribution of psoriatic arthritis within the hand can also differ from that of rheumatoid arthritis, in that two or three whole digits may be involved and the remaining ones spared, whereas in rheumatoid arthritis all MCP or PIP joints tend to be involved uniformly.
Enthesitis is inflammation at sites of bony insertion of tendons, ligaments, or joint capsules, and is the hallmark of these peripheral forms of spondyloarthropathy; in fact it is thought that most joint pathologic changes are the consequence of this inflammatory process at the enthesis. Thus, identification of enthesitis at MR imaging would suggest the diagnosis of spondyloarthropathy. MR imaging findings of enthesitis include diffuse bone marrow edema adjacent to the enthesis, as well as florid inflammatory soft-tissue changes at this site (Fig 6).
Other MR imaging findings of psoriatic arthritis include periostitis with thickening and contrast enhancement of the periosteum, and bone marrow edema observed in the diaphysis of the phalanges at a considerable distance from the subchondral bone and the capsular joint entheses.
In patients with rheumatoid arthritis, bone marrow edema usually occurs adjacent to cartilage in the subchondral bone and is much less extensive than in patients with spondyloarthropathy. Synovitis is not a predominant feature in most peripheral spondyloarthropathies. Moreover, whereas extensor tendons are more often involved than flexor tendons in rheumatoid arthritis, the opposite is true in psoriatic arthritis.
A key finding that may suggest the presence of spondylarthropathy is sacroiliitis, which is not a feature of RA. Imaging of the sacroiliac (SI) joints is frequently the first investigation if spondylarthropathy is suspected. The normal SI joint is composed of an anterior inferior cartilagenous portion that shows smooth margins and a posterior superior fibrous portion that shows irregular margins (Fig 7).
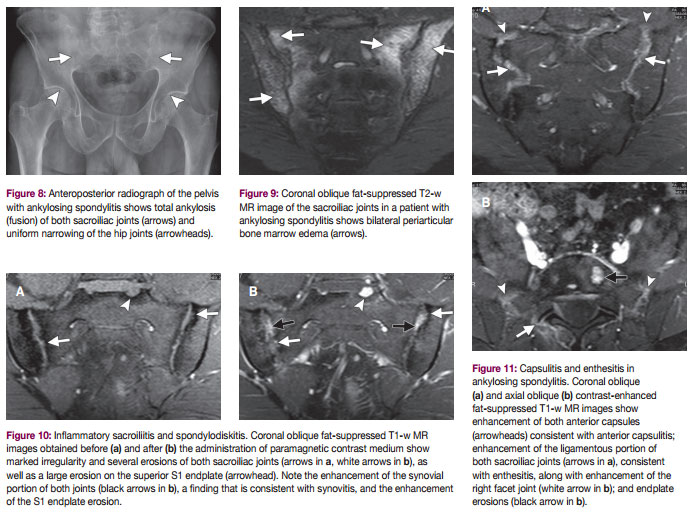
The anteroposterior radiograph of the pelvis is still the initial investigation performed in suspected spondylarthropathy, and erosions, illdefined margins, sacral-side sclerosis, narrowing or ankylosis of the SI joints are key albeit late features of the disease (Fig 8). This is particularly true if there is also hip involvement, which is present in 25% of cases.
Active inflammatory lesions in spondylarthropathy include bone marrow edema, synovitis, capsulitis, and enthesitis are best visualized on STIR, fat-suppressed T2-w, and contrast-enhanced fat-suppressed T1-w images (Fig 9-11). Bone marrow edema manifests with increased signal intensity on fat-saturated fast spinecho T2-w or STIR images, and with enhancement on gadolinium-enhanced fat-saturated fast spin-echo T1-w images. The presence of subchondral or periarticular bone marrow edema is mandatory for the definition of sacroiliitis at MR imaging.
The development of new MR sequences has revolutionized the interaction between MR imaging and treatment. A recent study has shown that diffusion-weighted and dynamic contrast-enhanced imaging may be effective in quantifying inflammatory changes at involved skeletal sites and, thus, useful for assessing treatment efficacy in ankylosing spondylitis.
In summary, MR imaging has revolutionised the management of RA and spondylarthropathy in that it allows much earlier detection of inflammatory joint changes and consequent early treatment to minimise joint damage. MR imaging, particularly with diffusion-weighted imaging and dynamic contrast– enhanced techniques, provides a quantitative assessment of the efficacy of treatment to help improve the outcome in these patients.