Advances In Oral Hormonal Contraception
Charles Savona-Ventura MD DScMed FRCOG AccrCOG MRCPI CLJ OMLJ
Consultant Obstetrician-Gynaecologist & Medical Historian
Down through the centuries, efforts to understand and to control fertility have been documented in almost every society. These efforts were two-edged: on one hand improving fertility to increase family size; on the other taking measures to prevent conception. Various Egyptian medical papyra describe methods for increasing fertility and for decreasing the likelihood of conception. The Industrial Revolution, beginning in the middle of the eighteenth century, resulted in dramatic changes in world economy. The resulting urbanisation brought on major problems of poverty, crowding and over-population with the attendant health hazards. By the beginning of the nineteenth century, the birth control movement had got under way first in Britain and subsequently in the United States. The methods of birth control available at the time included natural methods [prolonged lactation, the safe period and coitus interruptus]; barrier techniques [condom, cervical cap and diaphragm]; and surgical interventions [intrauterine device, abortion and sterilization]. Pre-twentieth century contraceptive methods known to have been used in Malta included prolonged lactation, coitus interruptus and abortion. These were generally frowned upon by the clergy and medical community alike.
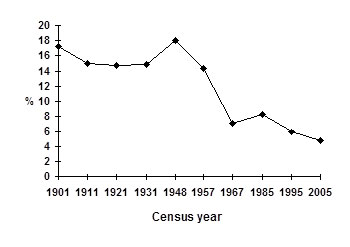
These methods obviously had their limitations. The post-Second World War social movement created a pressing need for an effective reversible contraceptive method that would allow women to delay their fertility while responding to the sexual revolution of the mid-twentieth century. The first orally active progestational agent, 17alpha-ethyltestosterone, had been synthesized by a Schering scientist, Hans H. Inhoffen, just before the beginning of World War II. This was to initiate the development of the first oral contraceptive pill and an ongoing programme to develop safer formulations. Dr Gregory Pincus, known as the ‘father of the pill’, together with John Rock and Celso Ramon Garcia tested the principle of hormonal inhibition of ovulation in 1951-1958. Their work led to the development of the effective hormonal contraceptive pill – Enovid in 1960. The scientists at Schering AG developed Anovlar using a highly effective progestogen and high dose oestrogen – 4 mg norethisterone acetate plus 0.05 mg ethinylestradiol – synthesised in Berlin and launched in 1961. The hormonal oral contraceptives were quickly introduced in Malta but were by 1967 being advertised as menstrual cycle regulators in the local medical press. However in spite of their availability on the local market, only 2% of the female population interviewed in 1971 were using hormonal contraception. By 1993, the usage rate had increased to 15.8%. The increasing use of contraception resulted in a definate drop in fertility rates over the second half of the twentieth century.
The increasing acceptance rate of the combined oral hormonal contraceptive pill was a multifaceted process linked partly to changing socio-religious norms on the Islands, but also the result of Schering’s ongoing quest to develop and market safer formulations with minimal side-effects. The first oral hormonal contraceptives were plagued with adverse media coverage because of the observed risks of increased incidence of thrombo-embolism and cardiovascular events. These effects were found to be oestrogen dose-dependant which resulted in a move to progressively reduce the dose of the ethinylestradiol component of the formulation from the original 0.05 mg. The traditional progestins, generally derived from either 19-norestosterone or 17alpha-hydroxyprogesterone, were associated with significant androgenic and anabolic side-effects that caused marked side-effects in susceptible individuals. Irrespective of the measures taken to reduce the dose in the various formulations, these medications continued to be associated with adverse effects and tolerability issues such as bleeding irregularities, nausea, acne, headaches and fluid retention-related symptoms such as bloating, breast tenderness and weight gain.
| Progestogenic | Glucocorticoid | Androgenic | Antiandrogenic | Antimineralocorticoid | |
| Progesterone | + | – | – | (+) | + |
| Drospirenone | + | – | – | + | + |
| Levonorgestrel | + | – | (+) | – | – |
| Gestodene | + | – | (+) | – | (+) |
| Norgestimate | + | – | (+) | – | – |
| Desogestrel | + | – | (+) | – | – |
| Dienogest | + | – | – | + | – |
| Cyproterone acetate | + | (+) | – | + | – |
Table 2: Pharmacological profiles of various progestins.
In view of these toleratibility issues, Schering continued its investigations to search for new progestagens with favourable clinical profiles. The result of this work was the novel progestin – drospirenone – a 17alpha-spirolactone derivative which has a unique pharmacological profile that, in addition to its potent progestogenic activity, has both antiandrogenic and antimineralocorticoid activities. Clinical studies with the oral contraceptive formulation containing 0.03 mg ethinylestradiol and 3 mg drospirenone (Yasmin) have demonstrated an excellent contraceptive efficacy and a good safety profile with an additional favourable impact on fluid retention-related symptoms, particularly fluid-related weight gain, wellbeing and acne and other skin-related problems. Yasmin was a success story, but its developers continued in their efforts towards making the formulation even safer by reducing the oestrogenic dose from 0.03 mg to 0.02 mg. To achieve this while retaining optimal contraceptive efficacy, the ethinylestradiol compound was bound within two molecules of betadex in order to improve the stability of ethinylestradiol at a lower dosage. In general, the pharmacokinetics and relative bioavailability of ethinylestradiol are unaffected by its inclusion within a betadex complex. This formulation containing 0.02 mg ethinylestradiol and 3 mg drospirenone has been recently launched under the tradename Yasminelle.
Clinical trials with Yasminelle have demostrated excellent contraceptive reliability with a pearl index of 0.23; improved emotional and physical well-being; stable body weight; reduction of acne lesions; good overall tolerance and non-significant changes in metabolic parameters. Patient satisfaction for Yasminelle reached 86.6%. Its main disadvantage over the higher dose ethinylestradiol formulations is that of an increased rate of intracycle bleeding – estimated at 20.8% for the first cycle and 5.1-11.3% in subsequent ones. This is mainly dependant on the overall patient weight and individual pharmacokinetics. Yasminelle therefore appears to be the best first-line oral contraceptive pill on the market today ensuring the delivery of a minimum dose of hormone to achieve the desired effect. Its progestogenic and antimineralocorticoid properties also make it highly tolerable with positive effects on weight, skin and PMS. If intracycle spotting persists or in women with a high BMI, then the patient can be upgraded to the 0.03 mg formulation – Yasmin.

