Ultrasound Assessment of right upper quadrant abdominal pain – Part II
Author : Dr Pierre Vassallo
Part 1 of this article discussed the importance of having an efficient diagnostic algorithm for right upper quadrant (RUQ) abdominal pain, since it is one of the most common presenting complaints to any clinic or emergency department. While acute cholecystitis is the most frequent cause of RUQ pain, more than a third of cases are due to other conditions. The same article also showed that abdominal ultrasound (US) is the imaging modality of choice because it is easily accessible, rapid, cost-effective, and safe since it involves no ionising radiation or potentially nephrotoxic intravenous contrast agent.1 Abdominal US visualises multiple upper abdominal organ systems that could be the source of the patient’s pain.
Part 1 of this article also described the US findings related to the biliary and hepatic causes of RUQ pain. The present Part 2 will discuss US findings seen with pancreatic and gastrointestinal causes, while a final forthcoming Part 3 will deal with adrenal, renal, thoracic and vascular causes of RUQ pain.
Pancreatic Causes of RUQ Pain
Pancreatitis usually presents with epigastric pain radiating to the back, but it may also present with RUQ pain. Pancreatitis is best imaged with computed tomography (CT) and magnetic resonance imaging (MRI). However, US is often the first investigation to suggest that there is a pancreatic problem particularly where symptoms are atypical.
Acute pancreatitis may be due to an obstructing gall stone, alcohol use or use of certain drugs such as steroids and sulpha-containing medications. It may also be idiopathic. Visualisation of the pancreas in US may be limited by an overlying gas-filled stomach or transverse colon. However, the head and neck of the pancreas are visible on US in most cases and acute pancreatitis can readily be detected and referred for further evaluation with CT or MRI.
In acute pancreatitis, the pancreas may appear enlarged, hypoechoic and shows ill-defined margins often with peripancreatic fluid collections. Pancreatitis may be focal (Fig 1a) and further evaluation with CT or MRI is needed to distinguish this entity from a pancreatic neoplasm. CT or MRI is also required to assess the extent of pancreatic damage as both exams distinguish viable (perfused) pancreatic segments from non-perfused/necrotic components (Fig 1b). Mesenteric vein thrombosis may complicate acute pancreatitis and may be seen on US. However, this complication may be more readily evident on CT or MRI (Fig 1c).3 In contrast, gall stones that could be causing the pancreatitis are more readily visualised with US.
Pancreatic cysts are asymptomatic in 70% of cases. They are mostly benign, and when they cause pain, are more likely to be malignant. Acute RUQ pain may be the presenting feature in case of intra-cyst haemorrhage, infection or secondary to obstruction of the pancreatic or biliary tree. Pancreatic cysts can be readily visualised with US if located in the head and neck of the pancreas (Fig 2). CT or MRI will usually be required to detect cysts located in the pancreatic body or tail; CT and MRI are more accurate for monitoring cyst size and for distinguishing cysts from tumours.
Pancreatic neoplasms may be solid or cystic. Adenocarcinomas are the most common solid tumours of the pancreas and are a leading cause of death due to tumor aggressiveness and often late diagnosis. Other solid pancreatic tumours include neuro-endocrine tumours, solid pseudopapillary tumours, pancreatic lymphoma and metastases. Cystic pancreatic neoplasms include serous cystadenomas, mucinous cystic neoplasms and intraductal papillary mucinous neoplasms.4
Since most pancreatic adenocarcinomas are in the pancreatic head, the typical clinical presentation is painless jaundice, which occurs due to obstruction of both pancreatic and biliary trees. Pain often develops late and is due to dorsal infiltration into the splanchnic plexus and the spine. On US, a pancreatic neoplasm generally appears as a hypoechoic and hypovascular mass (Fig 3a) that may impinge upon the portal venous vessels, the biliary tree and main pancreatic duct. Changes in the biliary and pancreatic ducts are best assessed with MR imaging using MRCP (magnetic resonance cholangio-pancreatography) sequences (Fig 3b). CT or MRI is required to evaluate vascular encasement as well as local and distant metastatic disease, all of which determine resectability of the tumour (Fig 3c).
GI causes of RUQ Pain
While many radiologists consider US as being of limited use for the analysis of the stomach and bowel, many gastrointestinal conditions are readily detected by US. These include neoplasms, bowel obstruction, bowel perforation, subacute appendicitis and hepatic flexure colitis.
In 14% of patients presenting in an emergency department with abdominal pain, the cause is subacute appendicitis. While the pain from a normally-located appendix usually presents around the umbilicus and the right iliac fossa, pain from a superiorly displaced appendix, such as may occur with a high-riding caecum, prior surgery or pregnancy, will be located in the RUQ. Acute appendicitis is the most common surgical emergency during pregnancy. Early detection is crucial as there is a 10-15% perforation rate with an associated 35-55% foetal mortality rate. US or MRI must be used to avoid exposure of the foetus to ionising radiation. Reported mean sensitivity and specificity of US for the detection of acute appendicitis during pregnancy is 87% and 97% respectively.5 The full thickness measurement (outer wall to outer wall) of a normal appendix should not exceed 7mm; thicknesses in excess of this, measured on US, are suggestive of appendicitis (Fig 4a). The appendix also shows a targetoid appearance (Fig 4b), absent peristalsis and non-compressibility on US. Tenderness over the appendix elicited by the compressing US probe is also a sign of appendicitis. US may also demonstrate an appendicolith, inflammation of the adjacent caecum and mesentery and para-appendiceal fluid. Abundant para-appendiceal fluid or a discontinuous wall of the appendix should raise the suspicion of perforation.
Hepatic flexure colitis, whether in isolation or as part of diffuse colitis, may result in RUQ pain; it may be due to infectious, inflammatory or ischaemic causes or as part of diverticular disease. On US, the normal anterior colonic wall is thin and abuts intestinal contents which are hyperechoic; the latter usually obscure the posterior wall due to dorsal shadowing (Fig 5a). Colitis leads to concentric thickening of the bowel wall with a central echogenic mucosal lining and a visible posterior wall (Fig 5b). Paracolic fluid may be present and the possibility of abscess formation must be considered. Distinction of infective colitis from that related to inflammatory bowel disease (e.g. Crohn’s disease or ulcerative colitis) is not possible based on US findings, but the clinical history and symptomatology my assist in distinguishing these entities. CT or MRI is more useful for detecting skip lesions, transmural extension of inflammation, strictures, fistulae and abscesses, which are characteristic of Crohn’s disease.
While diverticular disease is best diagnosed and its extent best assessed with CT or MRI, US may be the first step to detect an inflamed colonic diverticulum that presents with RUQ pain. Diverticulae are most common in the sigmoid colon (75%) with only 5% occurring in the ascending colon.6 However, an inflamed diverticulum close to the hepatic flexure of the colon will present with localised tenderness and can be detected on US (Fig 6).
Free peritoneal gas originating from a perforated visceral organ may be evident on US and should be actively sought in the presence of acute clinical peritoneal signs and a thickened visceral organ seen on US (Fig 7). Any suspicion of intestinal perforation should lead to further urgent evaluation with CT. CT will help to confirm the presence of free peritoneal gas and to identify the location and cause of the intestinal perforation. It will also distinguish free gas from gas in the bowel wall (pneumatosis intestinalis), which occurs in necrotizing enterocolitis due to bowel infection or ischaemia.
Conclusion
Pancreatic and gastrointestinal causes of RUQ pain are common, and their presence can be readily detected or at least suggested by US. Further evaluation with CT or MRI is often required to confirm the diagnosis and to detect complications. The next and final part of this article will discuss adrenal, renal, thoracic and vascular causes of RUQ pain.
References
- American College of Radiology. ACR Appropriateness Criteria: Right Upper Quadrant Pain. 1996. Updated 2013. Accessed January 26, 2018. Available from: https://acsearch.acr.org/docs/69474/Narrative/.
- Joshi, G et al. US of Right Upper Quadrant Pain in the Emergency Department: Diagnosing beyond Gallbladder and Biliary Disease. Radiographics 2018; 38(3):766-793.
- Case courtesy of Prof Frank Gaillard, Radiopaedia.org, rID: 18463.
- Sahani DV, Kadavigere R, Saokar A, et al. Cystic pancreatic lesions: a simple imaging-based classification system for guiding management. Radiographics2005; 25(6):1471–1484.
- Ledermann HP, Börner N, Strunk H, et al. Bowel wall thickening on transabdominal sonography. AJR Am J Roentgenol2000; 174(1):107–117.
- Peery AF, Keku TO, Martin CF, et al. Distribution and Characteristics of Colonic Diverticula in a United States Screening Population. Clin Gastroenterol Hepatol. 2016; 14(7):980-985.e1.
Figure Legends
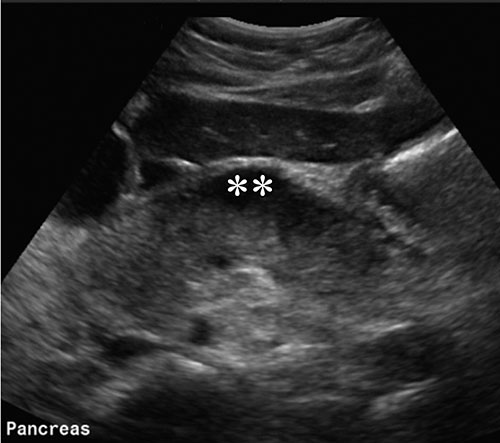
Figure 1a: Transverse US scan of the pancreas (**) showing a hypoechoic focus in the neck of the pancreas. This was confirmed on CT to be due to focal pancreatitis. CT or MRI is needed to distinguish focal pancreatitis from a pancreatic neoplasm and to assess the proportion of necrotic versus viable pancreatic tissue.

Figure 1b: Contrast-enhanced CT scan showing enhancing viable segments of the pancreas (P) from necrotic components/peripancreatic fluid (arrows).
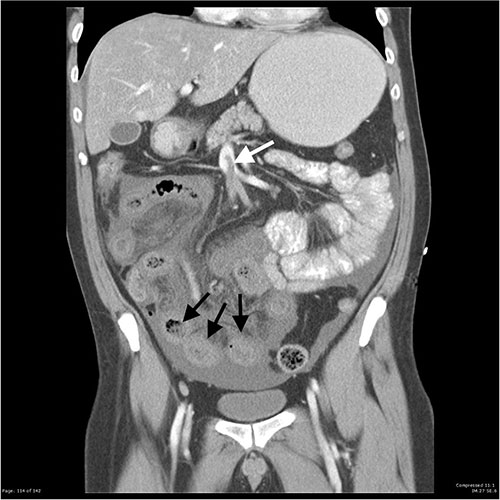
Figure 1c: Contrast-enhanced CT coronal reconstruction showing thrombus in the superior mesenteric vein (black arrow) and oedematous small bowel loops (white arrows).

Figure 2: Transverse abdominal US scan through the pancreas showing a small cyst in the pancreatic neck (arrow).

Figure 3a: Transverse US scan through the pancreas showing a pancreatic head tumour (T) with a dilated main pancreatic duct (PD). PV is the portal vein, SMA superior mesenteric vein and A aorta.

Figure 3b: MRCP sequence showing a dilated common bile duct (C) and main pancreatic duct (arrowheads). Abrupt obstruction of the main and pancreatic ducts (arrow) correlates with the site of the pancreatic head tumour.

Figure 3c: Transverse arterial-phase contrast-enhanced CT scan showing the coeliac artery (C) encased in tumour (arrows) that has spread by contiguous extension from a pancreatic neoplasm (not shown here).

Figure 4a: US scan through the long axis of an inflamed (thickened) appendix (arrows).

Figure 4b: US scan through the short axis of an inflamed appendix (arrows) demonstrating a targetoid appearance.

Figure 5a: Longitudinal US scan through a normal ascending colon. The anterior wall is thin and hypoechoic (arrows). Deep to the anterior wall, echogenic gas (*) obscures the posterior wall.

Figure 5b: Transverse US scan through the ascending colon showing a thickened bowel wall with central echogenic mucosa (targetoid appearance) and visibility of the posterior wall.

Figure 6: Transverse US scan through the RUQ showing the ascending colon (C) and an inflamed fluid-filled diverticulum (*) surrounded by inflamed echogenic omental fat (arrows). Tenderness was elicited during compression with the examining US probe.

Figure 7. Transverse US scan through the right hypochondrium showing the liver (L) and echogenic gas bubbles (arrows) between the liver and the diaphragm.

