Low breast density worsens prognosis in breast cancer
 Even though dense breast tissue is a risk factor for breast cancer, very low mammographic breast density is associated with a worse prognosis in breast cancer patients. Patient survival is affected only when low breast density is combined with an abundance of hyaluronan in the tumour, shows recent research from the University of Eastern Finland and Kuopio University Hospital.
Even though dense breast tissue is a risk factor for breast cancer, very low mammographic breast density is associated with a worse prognosis in breast cancer patients. Patient survival is affected only when low breast density is combined with an abundance of hyaluronan in the tumour, shows recent research from the University of Eastern Finland and Kuopio University Hospital.
The study also found that the existing Nottingham Prognostic Index for breast cancer can be improved by including low mammographic breast density and HER2 status in the index.
Breast cancer is the most common cancer in women and the leading cause of women’s cancer deaths. The main established prognostic factors are tumour size and differentiation grade, spreading to armpit lymph nodes, hormone receptor status and HER2-positivity.
However, there’s a need to define new and more accurate prognostic factors that could also allow for more personalised treatments.
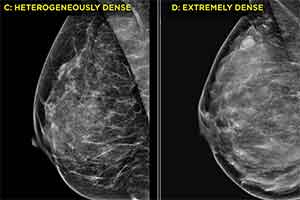
Mammographic breast density (MBD) has been a topic of research and discussion for decades. However, the focus has been mostly on the effect of MBD on screening sensitivity, masking effect and its status as a risk factor for breast cancer formation. Women with very dense breast tissue are known to have a 4- to 6-fold risk of breast cancer. The study concentrated on a less widely studied aspect of MBD – its prognostic effect in women who already have breast cancer.
In a study involving 278 breast cancer patients, researchers examined the prognostic value of MBD and mammographic tumour features and their relationship with the established prognostic factors. Very low MBD was found to be an independent prognostic factor for breast cancer. It was also associated with higher tumour grades and predicted worse survival.
Hyaluronan (HA) is a molecule naturally present in nearly all tissue types, but in cancer the metabolism of HA may change and promote the progression of cancer. The study also assessed the association between HA and its synthetizing enzymes with that of MBD and other mammographic and tumour characteristics. A strong link was found between low breast density and high expressions of HA and its synthesizing enzymes. Moreover, there was a dramatic reduction in patient survival exclusively when HA abundance was combined with low breast density.
In addition to very low MBD, HER2 positivity was also shown to be a prognostic factor for breast cancer, independent of the widely used Nottingham Prognostic Index (NPI). These factors were incorporated into a new prognostic index called the Kuopio-Nottingham Prognostic Index (KNPI), which has a higher predictive power than the original NPI.
According to Amro Masarwah, MBBS, who presented the results in his doctoral thesis, the findings suggest that dense breast tissue carries a more favourable prognosis and the mechanisms of cancer development are different from those of progression and aggressiveness.
“Since measuring density is becoming more common, physicians’ expertise with density will increase and this will open up doors for MBD to be used in patient outcome prediction.”
“Mammographic breast density is readily available, and can be easily measured and recorded at the time of diagnosis. Given the right training, excellent inter-reader agreement can be achieved and accurate measurements performed without the need of additional complicated, expensive and time consuming software or procedures,” Masarwah concludes.
“The new proposed cut-off definition of ‘fatty breasts’ might explain some of the discrepancies in the literature regarding the effects of density on prognosis,” he adds.
Source: University of Eastern Finland