Imaging Hamstring Injury
by Pierre Vassallo
MD PhD FACA Artz fur Radiologie
Consultant Radiologist
Increasing activity in the general population and the high demands placed on athletes have resulted in injuries to the hamstring muscle complex (HMC) being commonplace in sports. The HMC is by far the most frequently injured muscle and is often recalcitrant to even the most meticulous rehabilitation, making HMC injury a significant contributor to athletic morbidity. Knowledge of the HMC anatomy and of the spectrum of imaging findings in HMC injury will enable the musculoskeletal radiologist to make an accurate and useful contribution to the treatment of athletes at all levels of participation. For example tendon avulsion generally requires surgical reattachment, whereas strain patterns of injury are managed conservatively.
Magnetic resonance (MR) imaging and ultrasonography (US) are the imaging modalities of choice for HMC injury as they provide exquisitely detailed information with respect to localization and characterization of injury, assessment of severity and an indication of the prognosis. The portability and availability of US make it an attractive modality for the diagnosis of acute hamstring injuries, but its effectiveness is dependent on operator experience.
Imaging may not be necessary in all cases as clinical data may be enough to reach a diagnosis and decide on treatment. However, in those cases were the diagnosis is unclear or treatment is not achieving the expected results, imaging will provide valuable information about the nature of an injury and the effectiveness of treatment.
Differentiating between injury and muscle soreness, identifying recurrent tears in the rehabilitating athlete, or diagnosing an acute injury against a background of prior chronic strain can be difficult clinically. The latter situation is often clouded by the presence of scar tissue within the muscle. In these situations, imaging particularly with ultrasound is required.
The three muscles that constitute the HMC lie in the posterior compartment of the thigh and are the biceps femoris, semitendinosus, and semimembranosus muscles (Figure 1). The long head of the biceps femoris and the semitendinosus and semimembranosus muscles attach proximally to the ischial tuberosity (Figure 2). The short head of the biceps femoris originates from the posterior aspect of the femur and therefore does not cross the hip joint. The long and short heads of the biceps receive their nerve supply from two distinct nerves; this separate nerve supply may result in uncoordinated contraction of the two muscle segments and has been suggested as a cause for injury. The distal biceps femoris tendon inserts onto the head of the fibula, the lateral condyle of the tibia, and the fascia of the leg, a rather extensive attachment that is also thought to predispose it to tears. The distal insertions of the semitendinosus and semimembranosus muscles are at the medial aspect of the proximal tibia with extensions deep to the medial collateral ligament of the knee and in 50% of the population with an attachment to the posterior horn of the medial meniscus.
The HMC (or at least most of it) thus acts across two joints, namely the hip and the knee; when it contracts, it extends the hip and flexes the knee. Injury to the HMC occurs during contraction. There are two types of HMC contraction, eccentric and concentric contraction. Concentric contraction occurs during active combined hip extension and knee flexion. While eccentric contraction occurs to stablise (and protect) the knee joint during quadriceps activity; the quadriceps muscles, located in the anterior compartment of the thigh, oppose the HMC in that they cause combined hip flexion and knee extension. Almost all HMC injuries occur during eccentric activity when it contracts while it is being stretched. In addition, the strength of contraction of the HMC is only 60% that of the quadriceps muscles and this imbalance is thought to be a cause for injury. Any condition that diminishes the ability of a muscle to contract (eg, fatigue, weakness or even an old strain or tear) will make the muscle susceptible to injury because it impairs the muscle’s ability to absorb force. Thus, the benefits of adequate rest and an aggressive strengthening rehabilitation program cannot be overstated. Also at the microscopic level, the HMC is composed of a large proportion of type 2 “Fast-Switch” muscle fibres, which are capable to producing rapid tensile strength but are more susceptible to myofibrillar strain injury.
Even minor injury in the HMC results in ultrastructural change in which torn myofibrillar Z bands cause protein degradation with release of protein-bound ions leading to oedema; if this of sufficient magnitude, it can be visualized at imaging.
With minor injuries, microscopic analysis shows haemorrhage at these sites of disruption in the acute phase (<24 hours after disruption), followed by an inflammatory reaction whose time of occurrence is variable (usually at day 2) with laying down of fibrous tissue by day 7 to commence the formation of scar tissue. Such tissue first becomes visible as early as 14 days following initial insult, principally manifesting with low signal intensity on MRI and hypoechogenicity on US. At this point, the muscle has regained over 90% of its function. Nevertheless, given that fibrosis results in retraction, the optimal muscle length is altered, and, consequently, so is the ability of the muscle to maximally contract, which makes the HMC more susceptible to future injuries.
The most serious acute injury of the HMC is avulsion, which in adults usually involves the tendon but not the bone. This pattern of injury occurs more commonly at the ischial tuberosity than at the distal insertions. In such a case, avulsion almost always involves the conjoint tendon (biceps femoris and semitendinosus muscles) and often results in either complete or incomplete tearing of the semimembranosus (Figure 3). US may have difficulty visualising these injuries due to the depth the conjoint tendon beneath large gluteal muscles (especially in athletes). However, in most cases and with some examiner experience, even incomplete tears and common tendon degeneration can be readily visualised with ultrasound (Figure 4). Imaging allows accurate assessment of the degree of tendon retraction and of the tendon or bony edge for the surgeon contemplating primary surgical repair. In children, proximal avulsion more commonly involves bone with detachment of part of or the whole ischium, which has not yet fused with the other pelvic bones at the growth plate (Figure 5).
Distal avulsions are uncommon injuries but are most often seen in water skiers and football players. Avulsions of each tendon insertion have been reported, although avulsion of the semitendinosus is probably the most common (Figure 6). Avulsion usually occurs in the setting of prior or chronic injury, with abnormal tendon morphologic features or degeneration being the most likely predisposing factors. MR imaging accurately displays distal tendonous avulsion and the degree of retraction. However, US has superior spatial resolution, which, in combination with the superficial nature of the tendon, makes application of this modality ideal. Dynamic assessment, which is only possible with ultrasound can provide additional information about tendon integrity.
Partial tearing of the HMC is often referred to as a strain. Most strains occur in the region of the musculo-tendonous junction (MTJ) (Figure 2), which is the weakest link in the muscle complex. The MTJ is not a distinct area but a 10–12cm zone of transition in which muscle fibrils attach to the tendon. These tears can occur in any of the HMC muscles but are most common in the biceps femoris. On MR Imaging, the high signal intensity of oedema, fluid, and blood products characteristically dissects along disrupted fibrils creating a feathered appearance (Figure 7). The low echogenicity of muscle oedema is seen at US (Figures 8 & 9).
MR imaging and US are the imaging modalities of choice for assessing HMC injury. Experience, in combination with knowledge of the HMC anatomy, will assist the musculoskeletal radiologist in making an accurate and useful contribution to the treatment of athletes at all levels of participation.
Figure Legends
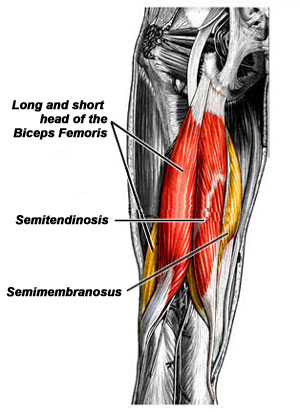
Figure 1. The HMC is composed of the semimembranosus, semitendinosus and the biceps femoris, the latter having two heads (long and short).
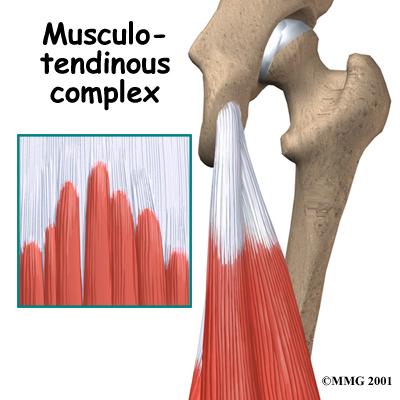
Figure 2. Proximal attachment of the HMC to the ischial tuberosity and composition of the MTJ.

Figure 3. Avulsion injury in a 29-year-old athlete with a hyperextension injury and persistent disability. Coronal MR image shows a large haematoma (*) with retracted fibres of the semitendinosus muscle and the long head of the biceps femoris tendon (straight arrow). The semimembranosus muscle (curved arrow) remains intact.

Figure 4. Sagittal US image shows degeneration of the proximal attachment of the HMC with loss of the normal bright fibrillar echotexture, heterogenous echoes, thickening (straight arrow) and fluid deep to the tendon (curved arrow). * = ischial tuberosity.

Figure 5. Old avulsion injury involving the right ischium that must have occurred prior to epiphyseal fusion.
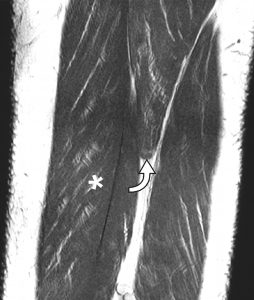
Figure 6. The patient presented with acute distal posterior knee pain during rehabilitation following ACL reconstruction. Coronal MR image shows avulsion of the semitendinosus tendon (arrow), with retraction of the muscle. The long head of the biceps femoris is located laterally (*), and the semimembranosus medially.
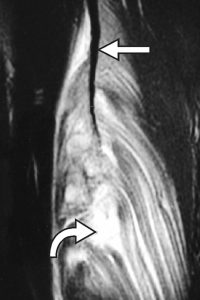
Figure 7. 26-year-old professional football player who presented with recurring hamstring strains and prolonged rehabilitation periods. Coronal MR image shows hyperintensity (curved arrow) in the MTJ of the biceps femoris in keeping with myofibrillar disruption and retraction from the central tendon slip (straight arrow).
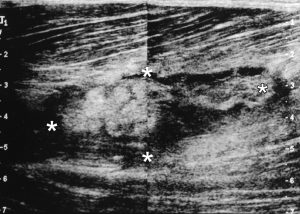
Figure 8. Sagittal US image demonstrates an abnormality with mixed echogenicity that corresponds to the MTJ disruption in the biceps femoris. * = boundaries of the area of disruption.
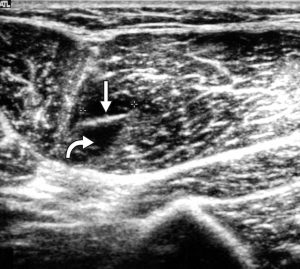
Figure 9. Transverse US image demonstrates oedema (curved arrow) around the MTJ (straight arrow) in the semitendinosus muscle.

